Home / Training / Manuals / Atlas of breast cancer early detection / Learning
.png)
Click on the pictures to magnify and display the legends

Click on this icon to display a case study
Atlas of breast cancer early detection
Filter by language: English / РусскийClinical breast examination (CBE) – Performing a breast examination |
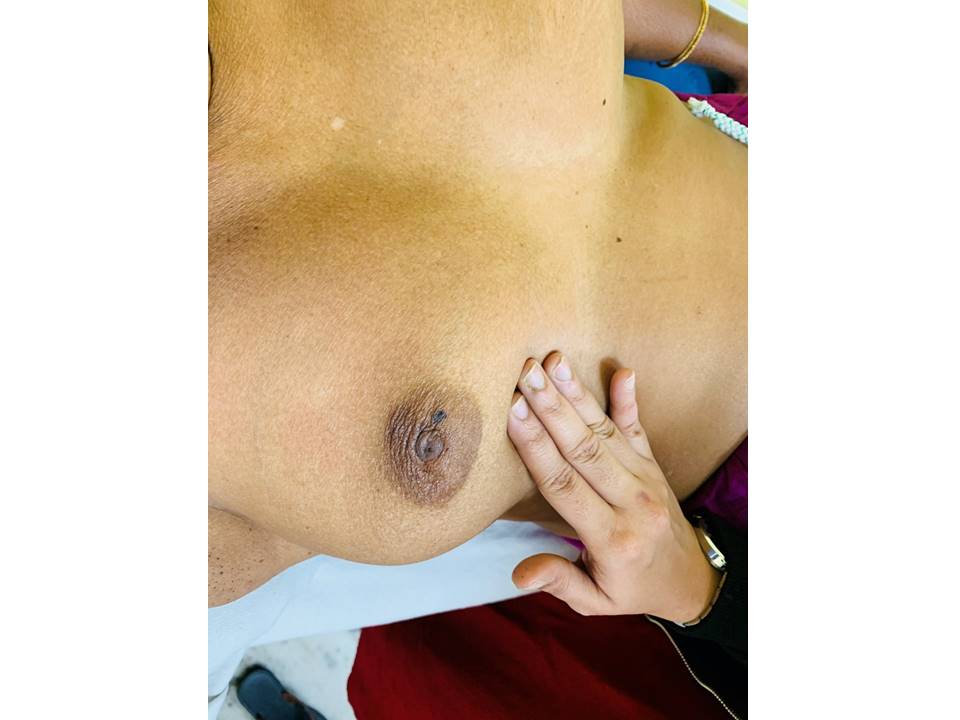
Clinical breast examination (CBE), also known as physical examination of the breast (PBE), is the systematic clinical examination of both the breasts, axillae and supraclavicular region to detect any abnormalities. Women with symptoms suggestive of breast cancer need to be appropriately evaluated with CBE by a trained primary care provider (e.g., a nurse or a clinician). Depending on the outcomes of CBE, diagnostic imaging (mammography and/or ultrasound of the breast) and FNAC or core biopsy are advised. A combination of CBE, diagnostic imaging and tissue diagnosis is referred to as “triple assessment”, which is also a key step in breast cancer screening pathway as all screen-positive women need to undergo these procedures. In addition to being a component of triple assessment, CBE is also recognized as a breast cancer screening test that is simple and feasible in limited resource settings. It can be provided by trained nurses or health workers and is less expensive compared with mammography-based screening programmes for populations. The steps of CBE are the same whether the procedure is performed in the context of screening or as a diagnostic evaluation. CBE involves the following steps:
Getting ready
Steps of inspection 1. Inspect both the breasts with the woman sitting comfortably with both arms resting on her thighs. 2. Repeat inspection with the woman pressing her hands into her hips so that the pectoralis muscles are contracted. 3. Ask the woman to place her hands behind her head and lean forward a little. Repeat the inspection. Look for the following abnormalities while you inspect the breasts:
Symmetry
Steps of palpation of the breasts and axillae Step 1. Palpate the breasts in the lying down position
Step 2. Palpate the breasts in the sitting position
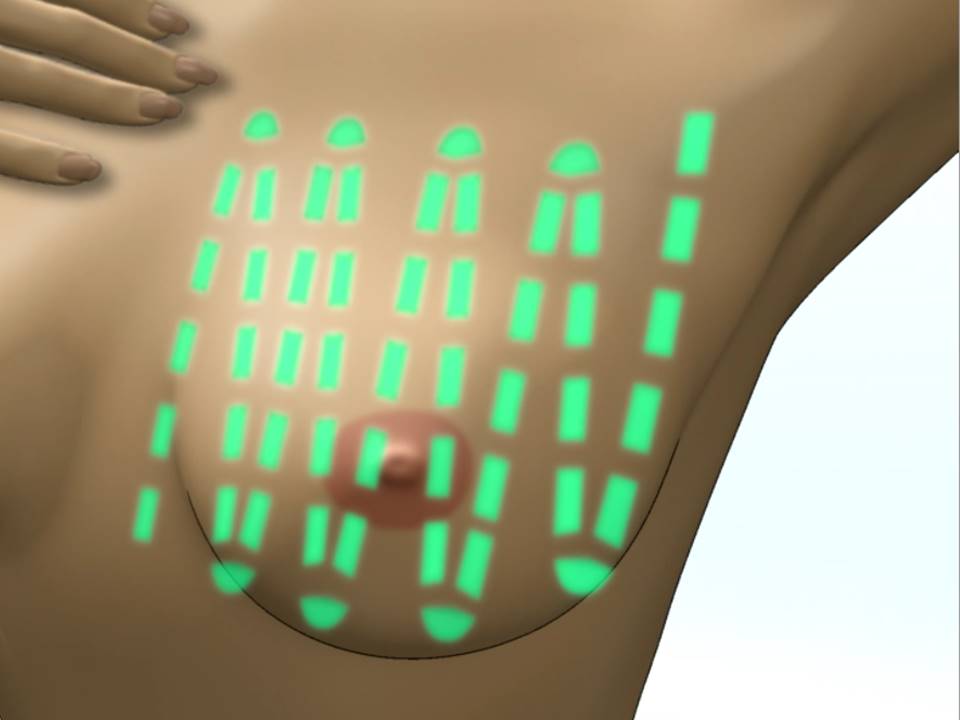
Linear method of breast palpation
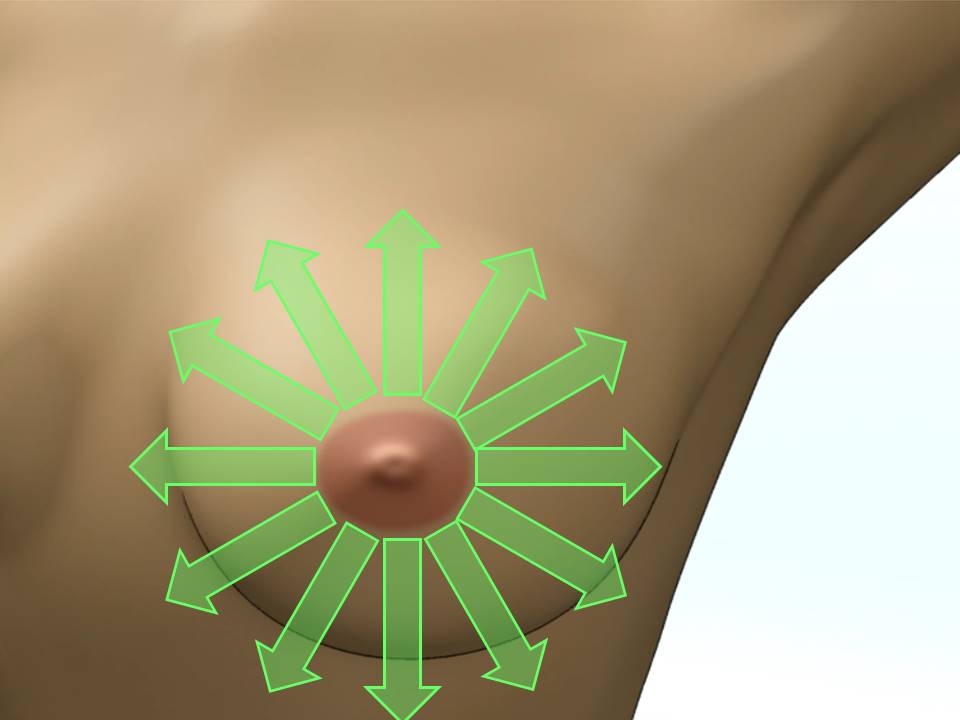
Dial of clock method of breast palpation The breast is visualized as the face of a clock and divided into areas accordingly. The 12 o’clock region is at the top centrally and the 6 o’clock region is at the bottom centre. The breast tissue is rolled in small circles starting from the nipple and radiating outwards. Start at 12 o’clock and continue clockwise or anticlockwise to return back to 12 o’clock. The entire breast tissue is thus systematically covered. Palpation of axilla Look for the following abnormalities while you palpate the breasts and the axilla:
Readers can download the step-by-step CBE examination checklist, which acts as a ready reckoner in the clinic. The checklist is also useful during a training programme to assess the trainee’s skill. |
Click on the pictures to magnify and display the legends
Click on this icon to display a case study
25 avenue Tony Garnier CS 90627 69366, LYON CEDEX 07 France - Tel: +33 (0)4 72 73 84 85
© IARC 2025 - Terms of use - Privacy Policy.
© IARC 2025 - Terms of use - Privacy Policy.