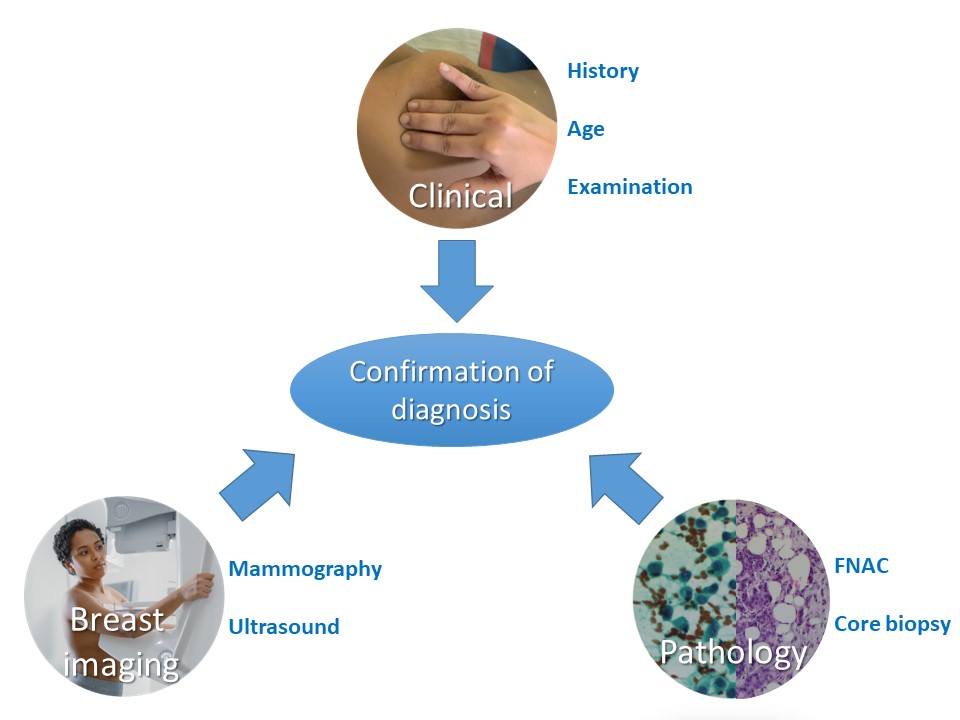
Core biopsy obtained with a needle (core needle biopsy) is the current standard of care for initial confirmation of diagnosis. It has the following advantages over FNAC:
However, FNAC is still highly relevant in settings with limited resources. Most lesions detected in such settings are clinically palpable and studies have shown that the sensitivity and specificity of FNAC from such lesions is marginally lower than that of core biopsy. Moreover, FNAC is rapid, logistically simpler, and can be organized in secondary care facilities. The patient does not have to travel to a tertiary care facility for the confirmation of diagnosis. This avoids any delay in diagnosis. The advantages and disadvantages of the two techniques are compared in detail in the following table.
|
FNAC |
Core needle biopsy |
Sampling procedure |
| Time taken |
Quicker procedure to perform without need for local anaesthesia |
Longer, local anaesthesia required |
| Training and expertise of staff |
Training is essential in aspiration and preparation of quality smears |
Training is essential and more intensive |
| Complications of procedure |
Less traumatic because needle bore is smaller (23/24G), so may be appropriate in women taking anticoagulants |
More traumatic because needle bore is larger (14/16G). Associated with potential complications such as haematoma, haemorrhage, and, very rarely, implantation of tumour cells along the needle track |
| Yield of material |
Repeated sampling and moving the needle in different directions yields more material for assessment |
Sampling limited to the tissue removed in the biopsy cores |
Diagnostic value in various breast lesions |
| Cystic lesions |
Indicated in the evaluation of cystic lesions of the breast, especially in ones with atypical imaging features |
Not useful in cystic lesions |
| Microcalcifications |
Inappropriate in assessment of microcalcifications detected on imaging because inadequate material may be aspirated from calcified areas |
Investigation of choice in evaluation of microcalcifications |
| DCIS |
Distinguishing between DCIS and invasive carcinoma is not possible because the cell morphology is similar in both |
Core biopsy, unlike FNAC, yields tissue fragments including architectural features, so it is possible to determine whether DCIS or invasive carcinoma is present |
| Papillary lesions |
Inaccurate for papillary lesions |
Useful to evaluate low-grade malignancies such as tubular carcinoma |
| Low-grade malignancies |
In the absence of architectural features, tumour cells with low-grade malignant features such as tubular carcinoma may be categorized as not malignant |
Useful to evaluate low-grade malignancies such as tubular carcinoma |
| Less-cellular breast lesions |
Not the sampling technique of choice for lesions that are relatively hypocellular and yield scanty epithelial material, such as sclerotic fibroadenomas, invasive breast carcinoma with extensive sclerosis, and infiltrating lobular carcinoma |
The diagnostic method of choice because the tissue section shows the sclerotic stromal tissue and intervening cell morphology |
Turnaround time |
Results are often available on the same day, possibly in a few hours |
Results are available after a few days. Tissue requires adequate fixation, then processing to make paraffin blocks and cutting before staining |
Cost of procedure |
Relatively inexpensive to perform |
More expensive than FNAC |
Effect of procedure on interpretation of subsequent histopathology of the lesion |
Does not significantly affect the subsequent histopathology of the sampled areas because of the small needle bore used |
For small lesions, the lesion seen on mammography may not be identified in subsequent open biopsy because it has been completely removed. The inflammation and fibrosis caused by the biopsy may interfere with the interpretation of subsequent excision biopsy, particularly with regard to grading and the estimation of the size of the lesion, especially in small lesions |
Biomarker status assessment |
Assessment of estrogen receptor (ER), progesterone receptor (PR), and human epidermal growth factor receptor 2 (HER2) status is not very reliable on cytology smears, although it is useful in cases of distant metastases and cases where tissue material is not available. However, on cell blocks with adequate cellularity, IHC is equivalent to a biopsy |
Assessment of ER, PR, and HER2 status is very reliable and is the standard practice |
.png)