Mammography
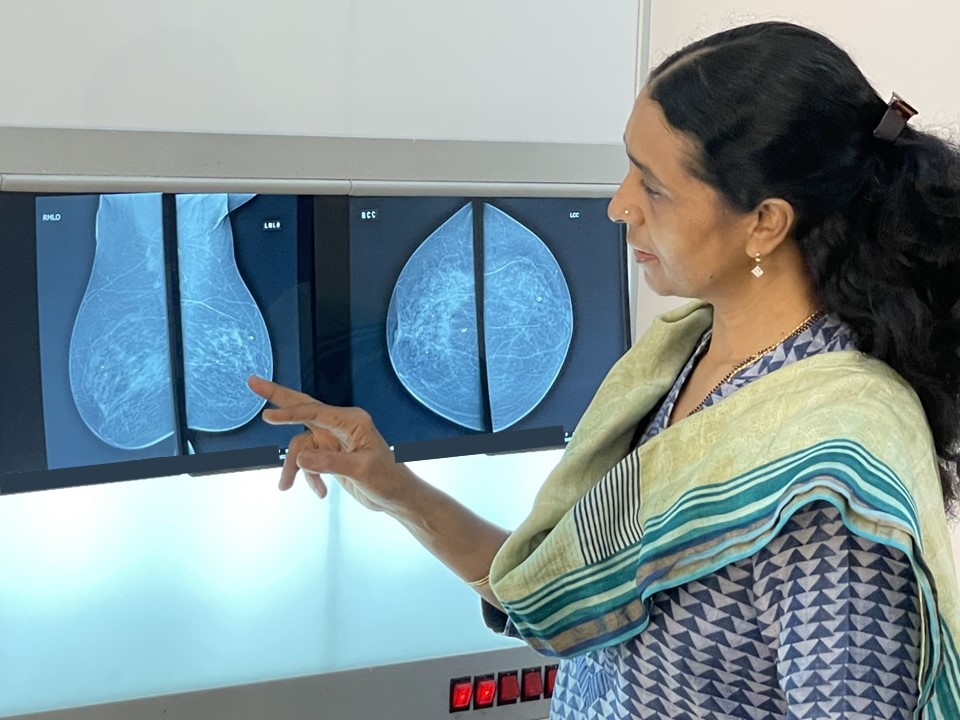
The technology of mammography has evolved over time. It includes screen-film and digital techniques.
Advantages of mammography
- Mammography remains the reference standard for the detection of breast abnormalities.
- Mammography screening is appropriate for early diagnosis of clinically occult breast cancer in asymptomatic women aged 45 years or older.
- It is the only modality of breast cancer screening proven to reduce breast cancer mortality rates in women aged 45–74 years.
- Diagnostic mammography has a sensitivity of more than 75% and a specificity of more than 90% for breast cancer detection. The sensitivity is low in women with dense breasts.
- The sensitivity of a breast cancer screening test is the percentage of women who have breast cancer (confirmed by the reference standard test of histopathology) that received a positive result on this test. A test with high sensitivity is good at detecting true positives.
- The specificity of a breast cancer screening test is the percentage of women who do not have breast cancer (confirmed by the reference standard test of histopathology) that received a negative result on this test. Specificity is a measure of how well a test can detect true negatives.
|
- The whole breast is examined in a single mammogram.
- Mammography enables comparison with previous mammograms and detects developing asymmetry.
- Mammography detects microcalcifications very efficiently.
Disadvantages of mammography
Mammography exposes the woman to radiation. The average radiation dose is less than 2 mGy for each breast. This dose is less than that received in a stand-alone chest X-ray. Having regular mammograms very slightly increases a woman’s chance of developing cancer over her lifetime.
- The equipment is expensive.
- Highly qualified medical staff (radiographers, radiologists, and medical physicists) are needed.
- Compression may be painful.
- A clinically occult cancer may be detected and treated just because of mammography screening. This cancer may never have grown, progressed, or caused symptoms. This is overdiagnosis. Between 10% and 15% of all cancers detected through mammography screening are said to be overdiagnosed.
- Mammography sensitivity is lower in dense breasts, which are commonly seen in young women.
Screen-film mammography
Screen-film mammography uses a molybdenum anode X-ray unit with a uniform-thickness breast-compression paddle to enable proper exposure of the breast tissue from chest wall to nipple. The image obtained on the single-emulsion film is developed and processed to get a visible image of the breast of optimal contrast and density.
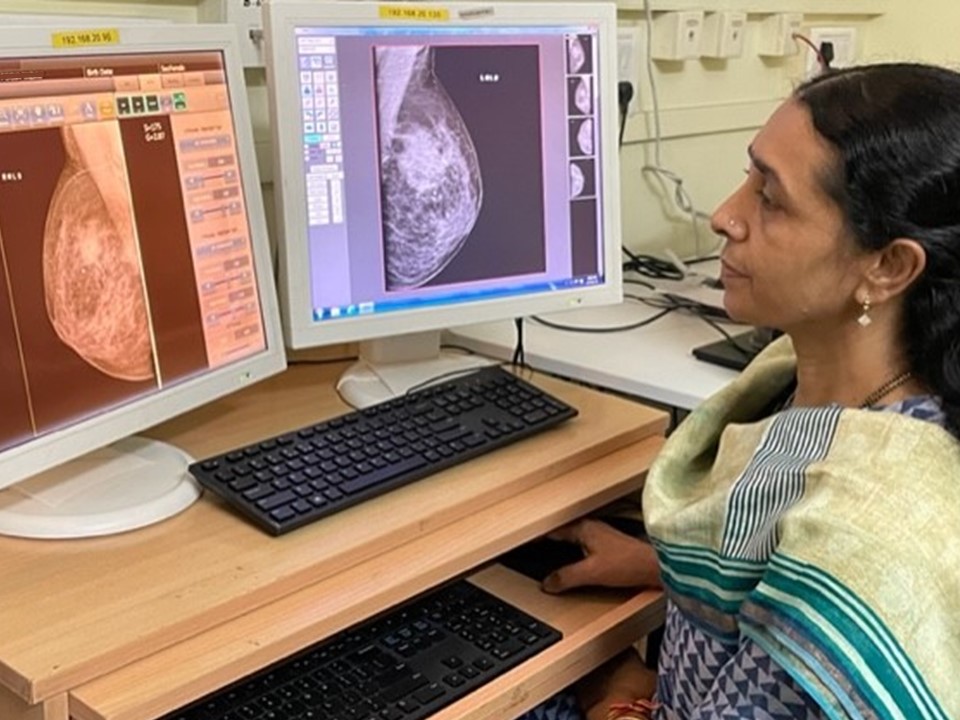
Full-field digital mammography (FFDM)
FFDM, more commonly known as digital mammography, has better contrast resolution than conventional mammography and enables optimization of both image acquisition and display. Screen-film mammography has better spatial resolution than FFDM, but FFDM has better contrast resolution, which overcomes the decreased spatial resolution. FFDM uses digital detectors that absorb X-ray photons and convert them into an electric charge, which is converted to an image. A computer processes the signal and displays the image on a high-resolution monitor, which can be viewed directly for interpretation. Digital images can be modified on the monitor to lighten or darken the image and to zoom in on certain sections to get a magnified view. Digital mammography has become the standard of care and has replaced screen-film mammography.
Computed radiography digital mammography (CR FFDM)
CR FFDM differs from FFDM in its image acquisition technology. Computed radiography is an indirect digital mammography technique that captures the image on a reusable plate. This reusable plate is then scanned by a reader to produce the digital image. CR FFDM and FFDM images can be either viewed on a monitor or printed and viewed for interpretation. Studies did not observe any advantages of CR FFDM over FFDM.
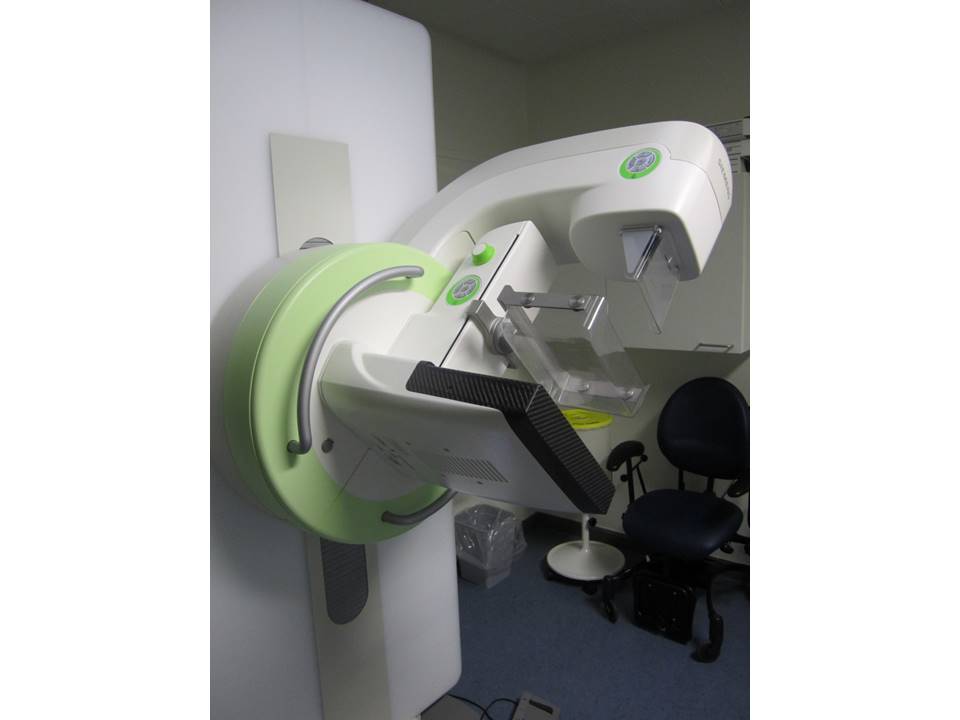
Digital breast tomosynthesis (DBT)
DBT represents a significant advance in technology and overcomes the inability of mammography to detect lesions hidden by dense overlapping fibroglandular breast tissues. DBT involves volumetric reconstruction of the whole breast from a finite number of low-dose two-dimensional projections obtained by different X-ray tube angles. The reconstructed images are presented on a high-resolution monitor using 0.5–1 mm slice separation. In DBT, morphological features for the detection of breast masses and breast calcifications are better defined, which makes diagnosis more accurate. The process is similar to computed tomography (CT) scan images of structures inside the body. Sequential visualization of thin images (slices) of the breast minimizes the masking effect of overlapping fibroglandular tissue and improves detection of a lesion or abnormality, particularly in dense breasts. DBT improves the accuracy of reporting, minimizes the number of unnecessary biopsies, and ensures that fewer women need to come back for a repeat mammogram.
Advantages of DBT
- DBT is a significant technological advance that overcomes the limitations of mammography when examining dense breasts.
- It can detect lesions hidden by the dense overlapping fibroglandular breast tissues by sequential visualization of thin images (slices) of the breast.
- DBT improves the accuracy of reporting in women with dense breasts, minimizes the number of unnecessary biopsies, and ensures that fewer women need to come back for a repeat mammogram, ultrasound, or MRI.
Disadvantages of DBT
- Women are exposed to higher levels of radiation in DBT. The dose used is approximately 2.2 times that used in digital mammography.
- The breast compression time is longer than in conventional digital mammography.
- The interpretation time for DBT is longer.
Breast ultrasound (hand-held)
Ultrasound is an imaging technique used to detect breast abnormalities using a high-frequency linear transducer on a high-resolution ultrasound machine. Introduced in the 1980s, breast ultrasound is commonly used as an adjunct to mammography, particularly to further evaluate women with dense breast tissues.
Advantages of breast ultrasound
- Breast ultrasound is the imaging modality of choice for the diagnosis of breast disease in women younger than 35 years.
- It is the imaging modality of choice to differentiate between solid and cystic lumps in the breast.
- It is used as an adjunct to mammography, particularly to further evaluate women with dense breast tissues.
- It is widely available.
- There is no radiation risk. It is safe to use to diagnose breast disease in pre- and postpubertal girls, pregnant women, and lactating mothers.
- There is no discomfort during the procedure and breast compression is not required.
- It can be used to assess breast tissue when breast implants are present.
- Ultrasound-guided interventions, both diagnostic and therapeutic, are widely used.
Disadvantages of breast ultrasound
- Trained expertise is necessary because the procedure is operator-dependent.
- Microcalcifications cannot be characterized by ultrasound.
- Sensitivity may be lower in large breasts.
- It is not recommended as a breast cancer screening modality.
Automated breast ultrasound (ABUS)
ABUS is a breast ultrasound technique in which image acquisition is separated from interpretation. A trained nurse or technician applies the transducers in the right positions and keeps gentle pressure on the breast tissue while the breast is scanned craniocaudally and mediolaterally. The radiologist reviews the entire set of images, which are stored digitally on a dedicated workstation. Because breast image acquisition is minimally operator-dependent, consistency in identifying suspicious lesions is improved. Several types of ABUS are available, with different designs, image acquisition approaches, and workstation features. Dedicated computer-aided detection software for ABUS has the potential to create three-dimensional images.
Conventional hand-held breast ultrasound is very operator-dependent and requires considerable time for the radiologist to assess both breasts. In contrast, ABUS is less operator-dependent, requires less time from a radiologist, and has more reproducible results. In September 2012, the United States Food and Drug Administration approved ABUS for screening women with dense breasts after negative findings on mammography. One multicentre cross-sectional study was carried out in China in 2016 to compare the diagnostic performance of hand-held breast ultrasound, ABUS, and mammography. A total of 1974 women aged 30–69 years were recruited. The results suggested that the clinical performance of ABUS was comparable with that of hand-held ultrasound for breast cancer detection, and that both traditional ultrasound and ABUS have better performance than mammography, especially among women with high-density breasts.
Advantages of ABUS
- ABUS is less operator-dependent than conventional breast ultrasound.
- It requires less radiologist time.
- The results are more reproducible.
- Three-dimensional images can be produced.
Disadvantages of ABUS
Breast MRI
Breast MRI is primarily a supplemental tool for breast imaging used along with mammography and/or breast ultrasound. The sensitivity of contrast-enhanced breast MRI in the detection of cancer is considerably higher than that of either mammography or ultrasound. MRI is the screening modality of choice for women at high lifetime risk of breast cancer, such as those with mutations in the
BRCA1 and/or
BRCA2 genes.
Advantages of breast MRI
- Breast MRI is a supplemental tool for breast imaging along with mammography and/or breast ultrasound.
- It does not involve radiation.
- Because MRI has 90–100% sensitivity, it is recommended for evaluation of multicentricity or bilaterality of the disease in a known case of breast cancer.
- Its high sensitivity makes it the breast imaging modality of choice for women at high lifetime risk of developing breast cancer.
- It can be used to evaluate possible rupture of silicone breast implants.
Disadvantages of breast MRI
- Lack of availability and high cost of investigation limit widespread use of MRI, especially as a screening modality.
- MRI is not advised for women with devices in their bodies that are not compatible with MRI (for example: cardiac pacemakers, implantable cardioverter defibrillators (ICDs) and cardiac resynchronization therapy (CRT) devices, cochlear implant, metallic foreign body in the eye) or for women with kyphoscoliosis who cannot lie prone.
- MRI cannot be performed in women with compromised renal function and those allergic to MRI contrast agents.
.png)