Home / Training / Manuals / Atlas of breast cancer early detection / Cases
Atlas of breast cancer early detection
Filter by language: English / Русский
Go back to the list of case studies
.png) Click on the pictures to magnify and display the legends
Click on the pictures to magnify and display the legends
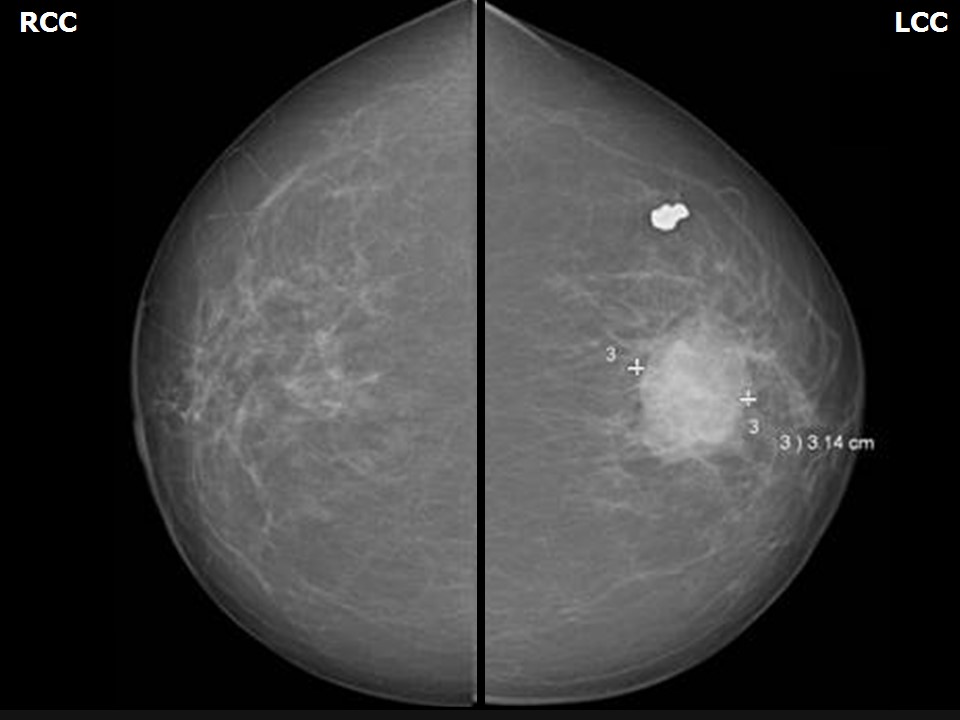
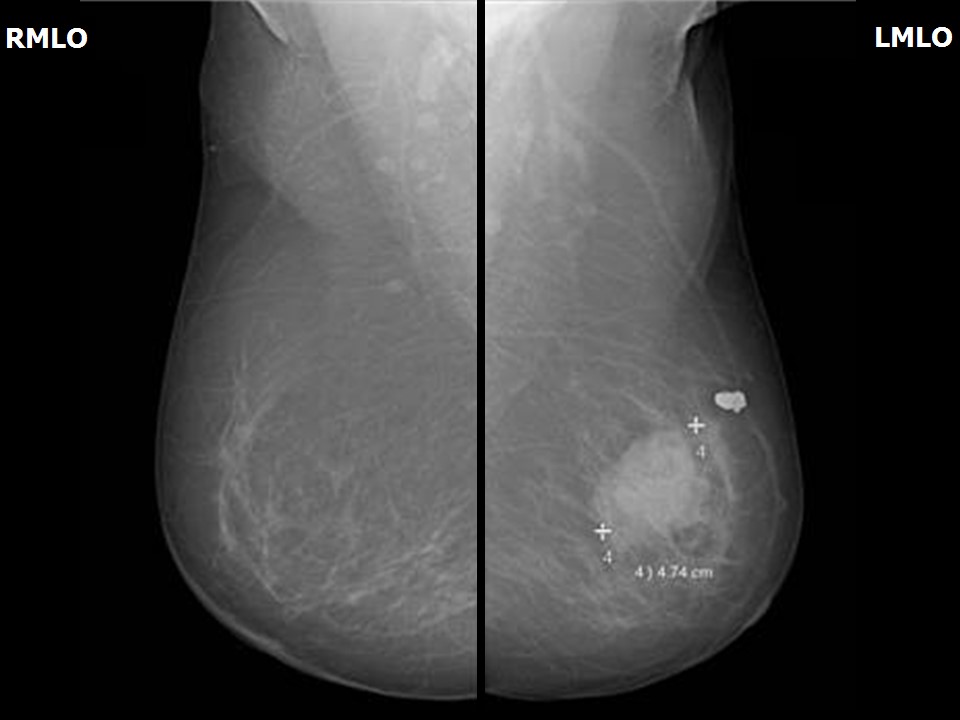
BI-RADS Category (2013, left): 5 (highly suggestive of malignancy)
BI-RADS Category (2014, right): 4B (moderate suspicion of malignancy)
BI-RADS Category (2017, right): 5 (highly suggestive of malignancy)
| Case number: | 120 |
| Age: | 75 |
| Clinical presentation: | Postmenopausal woman who had undergone an MRM for left breast cancer 4 years ago and was on regular follow-up presented for mammography screening. Clinical examination of the right breast was found to be normal. |
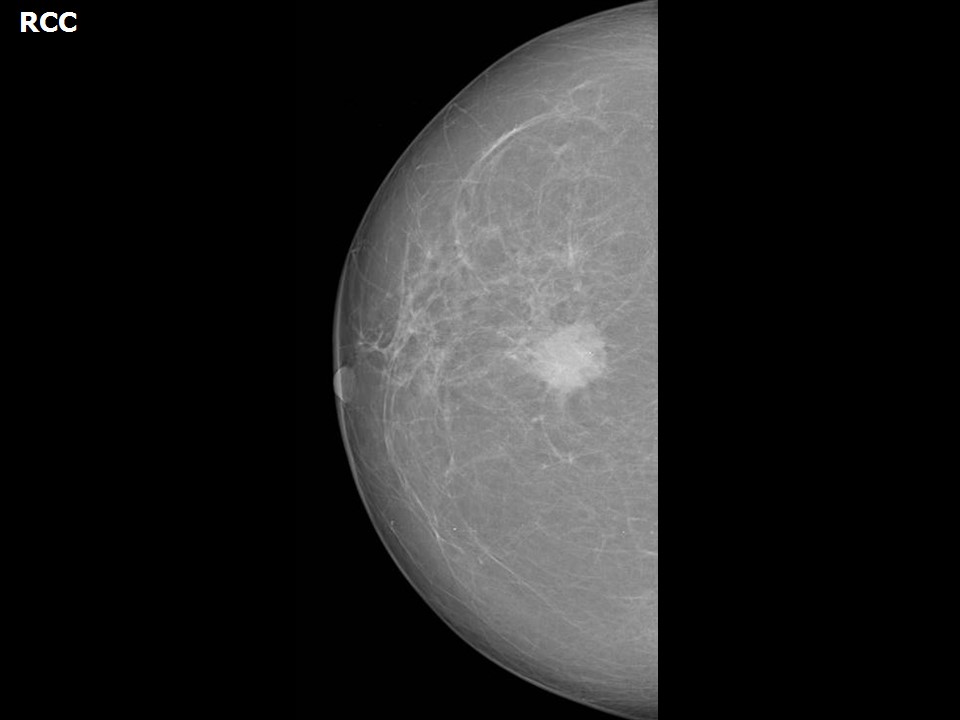
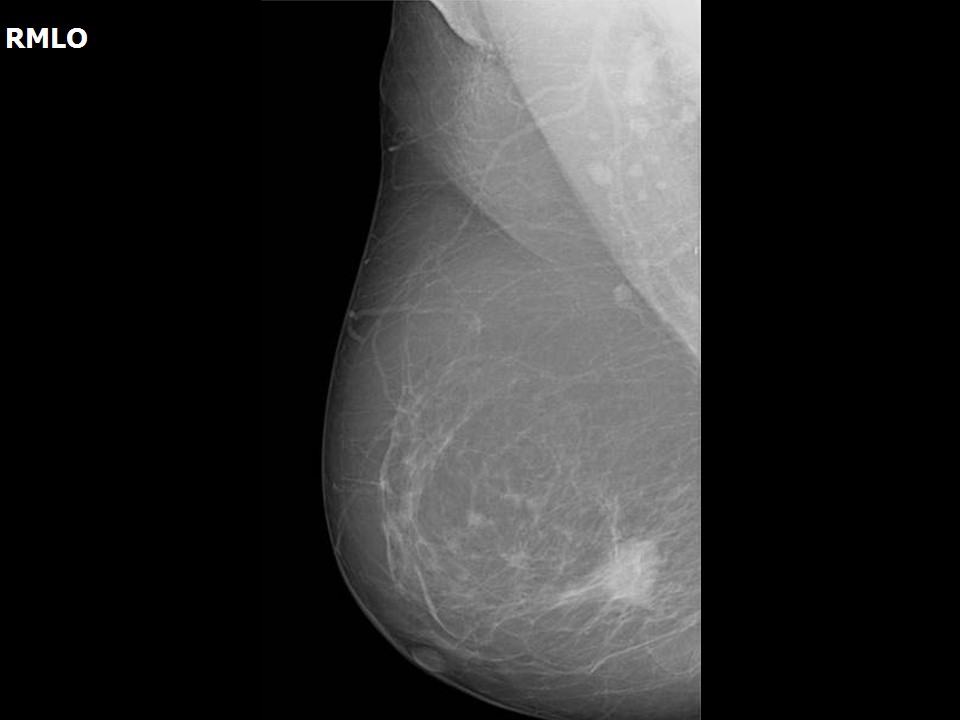
Mammography:
| Breast composition: | ACR category a (the breasts are almost entirely fatty) | Mammography features: |
| ‣ Location of the lesion: | May 2013: Left breast, central portion of the breast at 12 o’clock, middle third |
| ‣ Mass: | |
| • Number: | 1 |
| • Size: | 4.7 × 3.1 cm |
| • Shape: | Irregular |
| • Margins: | Indistinct |
| • Density: | High |
| ‣ Calcifications: | |
| • Typically benign: | None |
| • Suspicious: | None |
| • Distribution: | None |
| ‣ Architectural distortion: | Present |
| ‣ Asymmetry: | None |
| ‣ Intramammary node: | None |
| ‣ Skin lesion: | None |
| ‣ Solitary dilated duct: | None |
| ‣ Associated features: | Architectural distortion and trabecular thickening |
| Breast composition: | ACR category a (the breasts are almost entirely fatty) | Mammography features: |
| ‣ Location of the lesion: | May 2013: Left breast, upper outer quadrant at 2 o’clock, middle third |
| ‣ Mass: | |
| • Number: | 1 (calcified mass) |
| • Size: | 1.0 cm in greatest dimension |
| • Shape: | Irregular |
| • Margins: | Circumscribed |
| • Density: | Calcified mass |
| ‣ Calcifications: | |
| • Typically benign: | Coarse |
| • Suspicious: | None |
| • Distribution: | None |
| ‣ Architectural distortion: | None |
| ‣ Asymmetry: | None |
| ‣ Intramammary node: | None |
| ‣ Skin lesion: | None |
| ‣ Solitary dilated duct: | None |
| ‣ Associated features: | None |
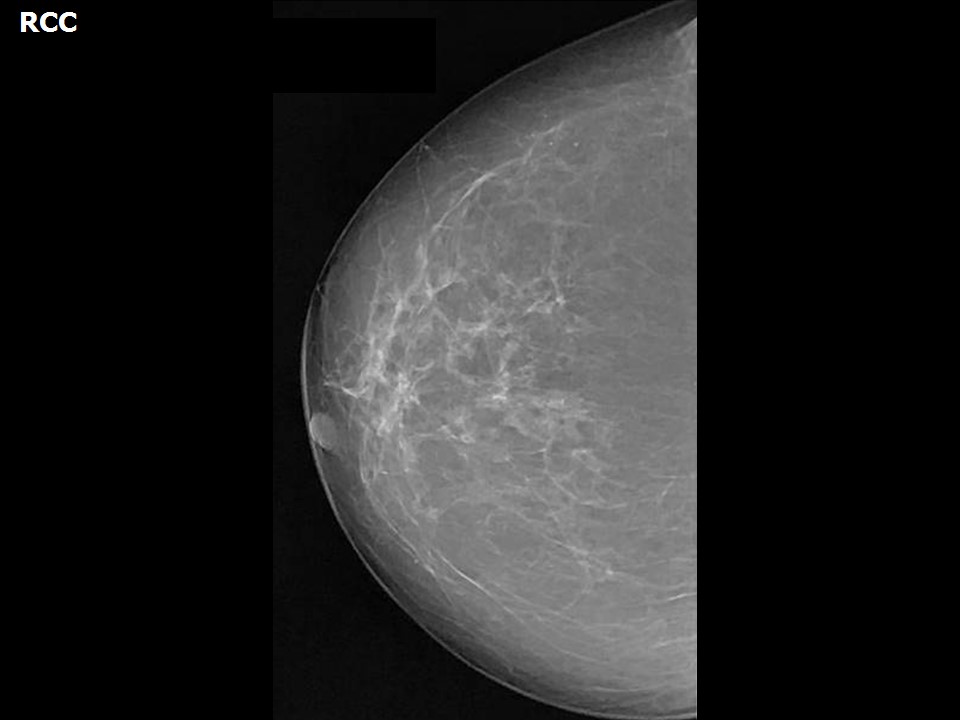
| Breast composition: | ACR category a (the breasts are almost entirely fatty) | Mammography features: |
| ‣ Location of the lesion: | May 2013: Right breast, lower quadrants at 6 o’clock, posterior third |
| ‣ Mass: | |
| • Number: | 1 |
| • Size: | None |
| • Shape: | None |
| • Margins: | None |
| • Density: | None |
| ‣ Calcifications: | |
| • Typically benign: | None |
| • Suspicious: | Microcalcification |
| • Distribution: | Grouped |
| ‣ Architectural distortion: | None |
| ‣ Asymmetry: | None |
| ‣ Intramammary node: | None |
| ‣ Skin lesion: | None |
| ‣ Solitary dilated duct: | None |
| ‣ Associated features: | None |
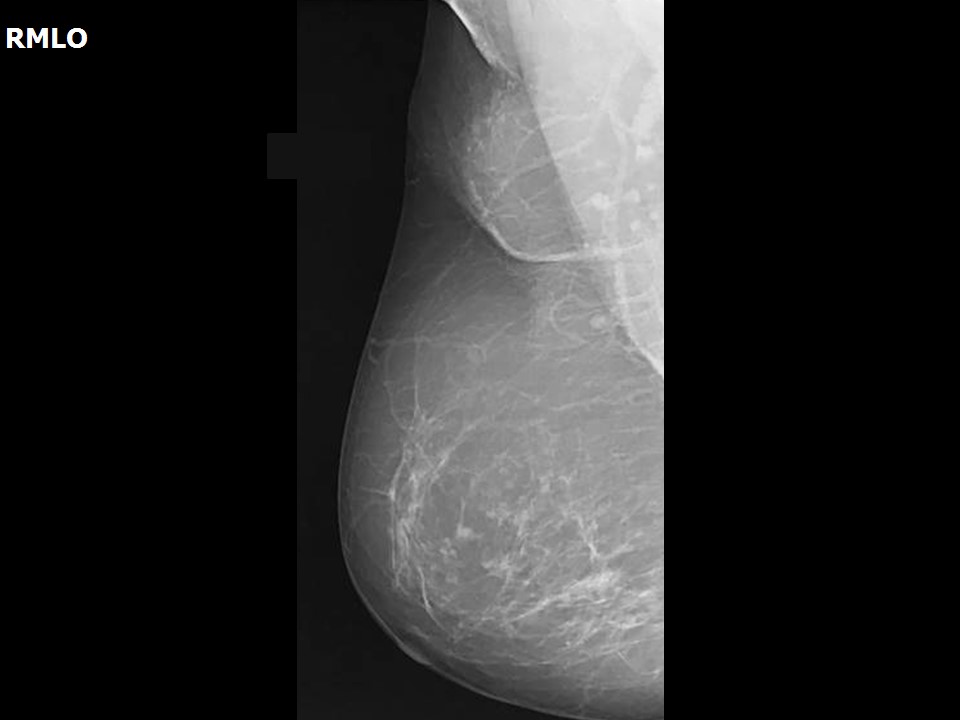
| Breast composition: | ACR category a (the breasts are almost entirely fatty) | Mammography features: |
| ‣ Location of the lesion: | 2014: Right breast, lower quadrants at 6 o’clock, posterior third |
| ‣ Mass: | |
| • Number: | 1 (this is the developing asymmetry) |
| • Size: | 0 |
| • Shape: | None |
| • Margins: | None |
| • Density: | None |
| ‣ Calcifications: | |
| • Typically benign: | None |
| • Suspicious: | Fine microcalcifications |
| • Distribution: | Grouped |
| ‣ Architectural distortion: | None |
| ‣ Asymmetry: | Focal |
| ‣ Intramammary node: | None |
| ‣ Skin lesion: | None |
| ‣ Solitary dilated duct: | None |
| ‣ Associated features: | None |
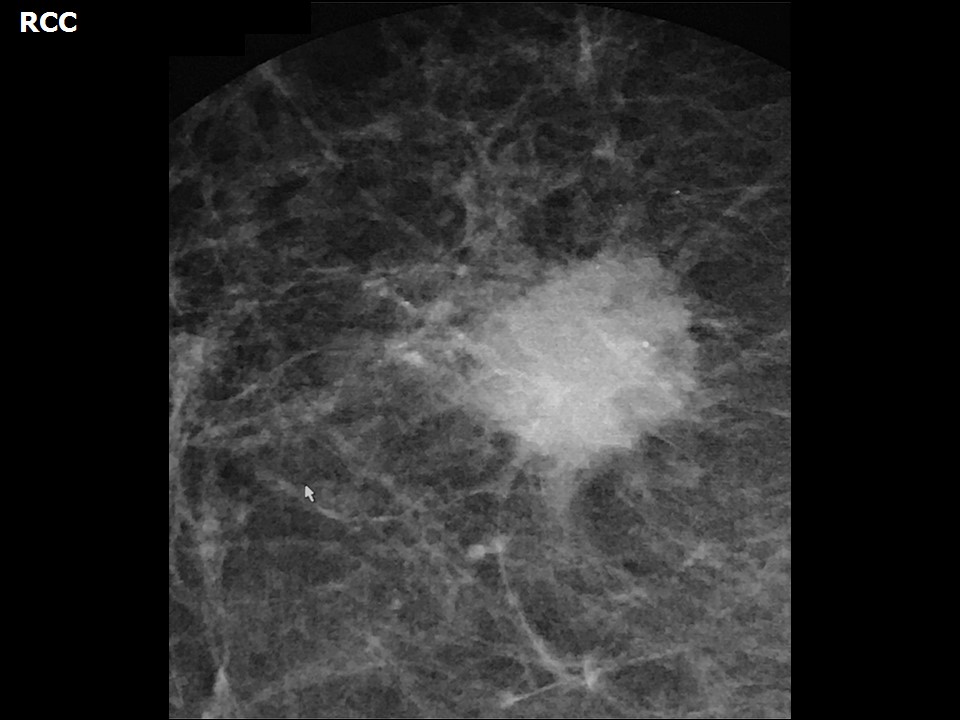
| Breast composition: | ACR category a (the breasts are almost entirely fatty) | Mammography features: |
| ‣ Location of the lesion: | 2017: Right breast, lower quadrants at 6 o’clock, posterior third |
| ‣ Mass: | |
| • Number: | 1 (this is the developing asymmetry) |
| • Size: | 1.4 × 1.0 cm |
| • Shape: | Irregular |
| • Margins: | Spiculated |
| • Density: | High |
| ‣ Calcifications: | |
| • Typically benign: | None |
| • Suspicious: | Fine pleomorphic |
| • Distribution: | None |
| ‣ Architectural distortion: | None |
| ‣ Asymmetry: | Developing asymmetry |
| ‣ Intramammary node: | None |
| ‣ Skin lesion: | None |
| ‣ Solitary dilated duct: | None |
| ‣ Associated features: | Calcifications |
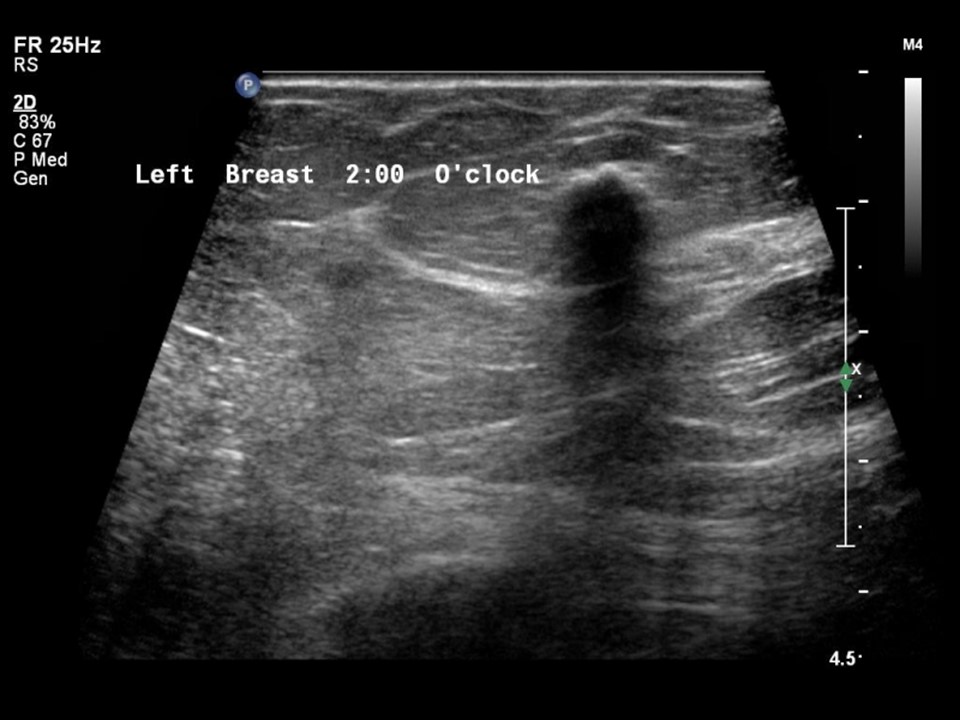
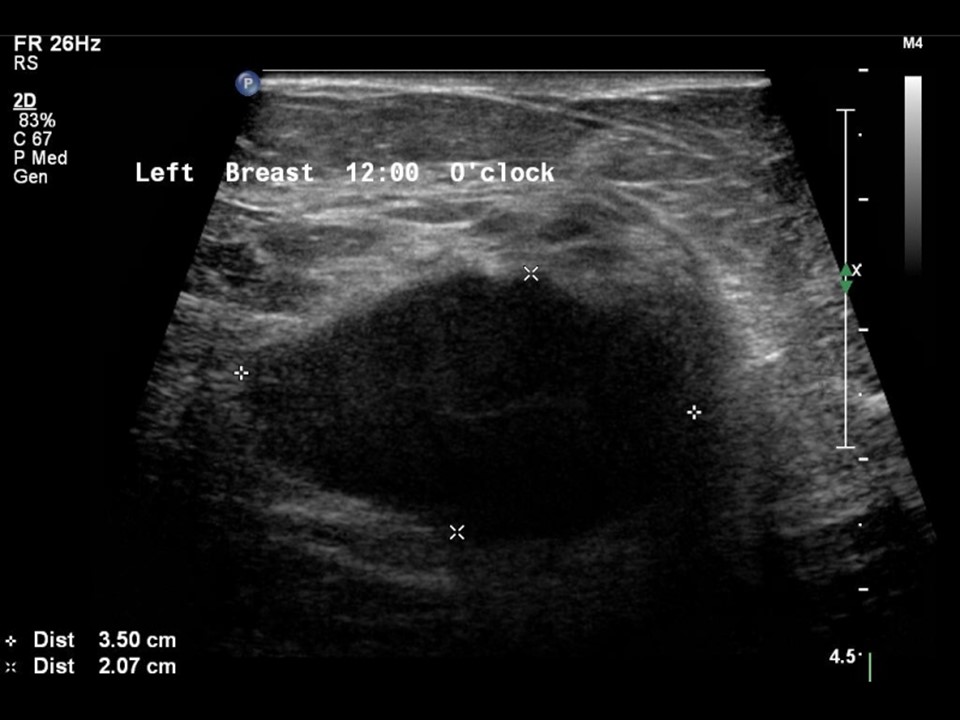
Ultrasound:
| Ultrasound features: 2013: Left breast, upper outer quadrant at 10 o'clock | |
| ‣ Mass | |
| • Location: | 2013: Left breast, upper outer quadrant at 10 o'clock |
| • Number: | 1 |
| • Size: | 3.5 × 2.0 cm |
| • Shape: | Irregular |
| • Orientation: | Parallel |
| • Margins: | Indistinct |
| • Echo pattern: | Hypoechoic |
| • Posterior features: | No posterior features |
| ‣ Calcifications: | None |
| ‣ Associated features: | None |
| ‣ Special cases: | None |
| Ultrasound features: 2013: Left breast, upper outer quadrant at 2 o'clock | |
| ‣ Mass | |
| • Location: | 2013: Left breast, upper outer quadrant at 2 o'clock |
| • Number: | 1 (calcified lesion) |
| • Size: | 0.7 cm in greatest dimension |
| • Shape: | Oval |
| • Orientation: | Parallel |
| • Margins: | Circumscribed |
| • Echo pattern: | Hypoechoic |
| • Posterior features: | Strong posterior shadowing |
| ‣ Calcifications: | Calcified density |
| ‣ Associated features: | None |
| ‣ Special cases: | None |
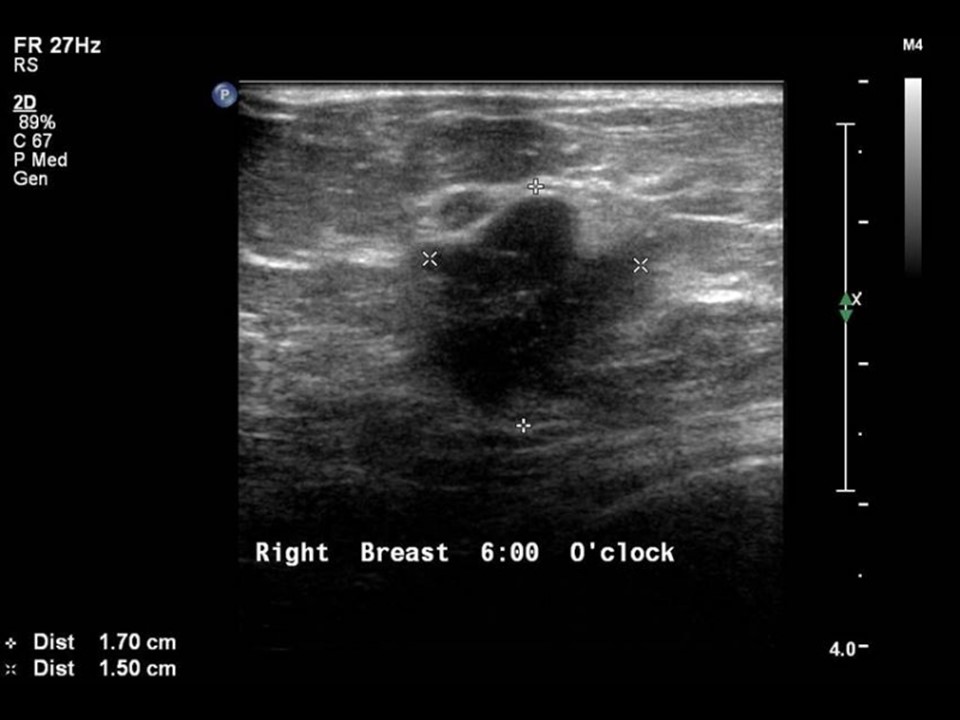
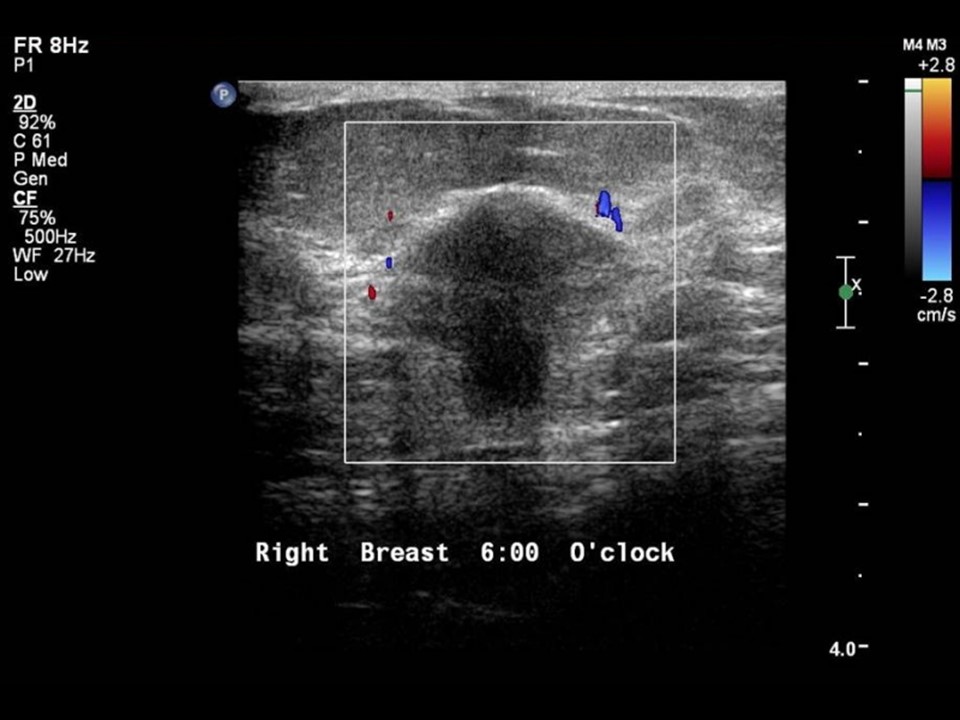
| Ultrasound features: 2017: Right breast, lower quadrants at 6 o’clock, 2.2 cm from nipple, 1.0 cm skin depth | |
| ‣ Mass | |
| • Location: | 2017: Right breast, lower quadrants at 6 o’clock, 2.2 cm from nipple, 1.0 cm skin depth |
| • Number: | 1 (this is a developing asymmetry) |
| • Size: | 1.7 × 1.5 cm |
| • Shape: | Irregular |
| • Orientation: | Not parallel |
| • Margins: | Indistinct |
| • Echo pattern: | Hypoechoic |
| • Posterior features: | No posterior features |
| ‣ Calcifications: | Macrocalcifications in mass |
| ‣ Associated features: | Internal vascularity |
| ‣ Special cases: | None |
| Ultrasound features: 2017: Right breast, lower quadrants at 6 o’clock, superolateral to primary lesion | |
| ‣ Mass | |
| • Location: | 2017: Right breast, lower quadrants at 6 o’clock, superolateral to primary lesion |
| • Number: | 1 (this is a developing asymmetry, multicentric focus) |
| • Size: | 0.5 cm in greatest dimension |
| • Shape: | Oval |
| • Orientation: | Parallel |
| • Margins: | Indistinct |
| • Echo pattern: | Hypoechoic within solitary dilated duct |
| • Posterior features: | No posterior features |
| ‣ Calcifications: | None |
| ‣ Associated features: | Duct changes |
| ‣ Special cases: | None |
BI-RADS:
BI-RADS Category (2013, right): 3 (probably benign)BI-RADS Category (2013, left): 5 (highly suggestive of malignancy)
BI-RADS Category (2014, right): 4B (moderate suspicion of malignancy)
BI-RADS Category (2017, right): 5 (highly suggestive of malignancy)
Further assessment:
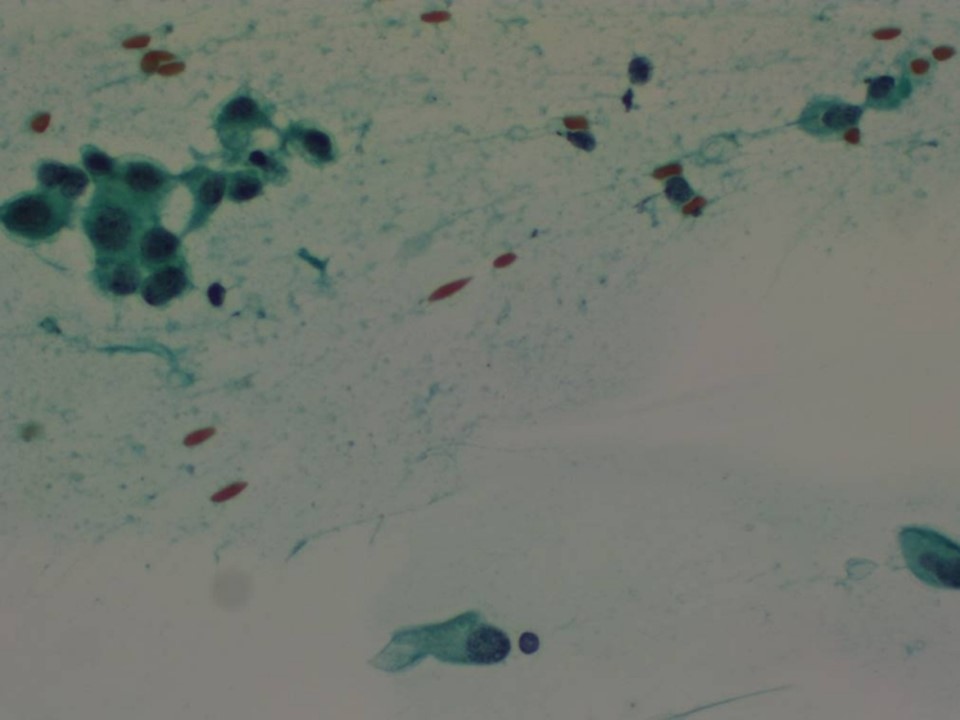
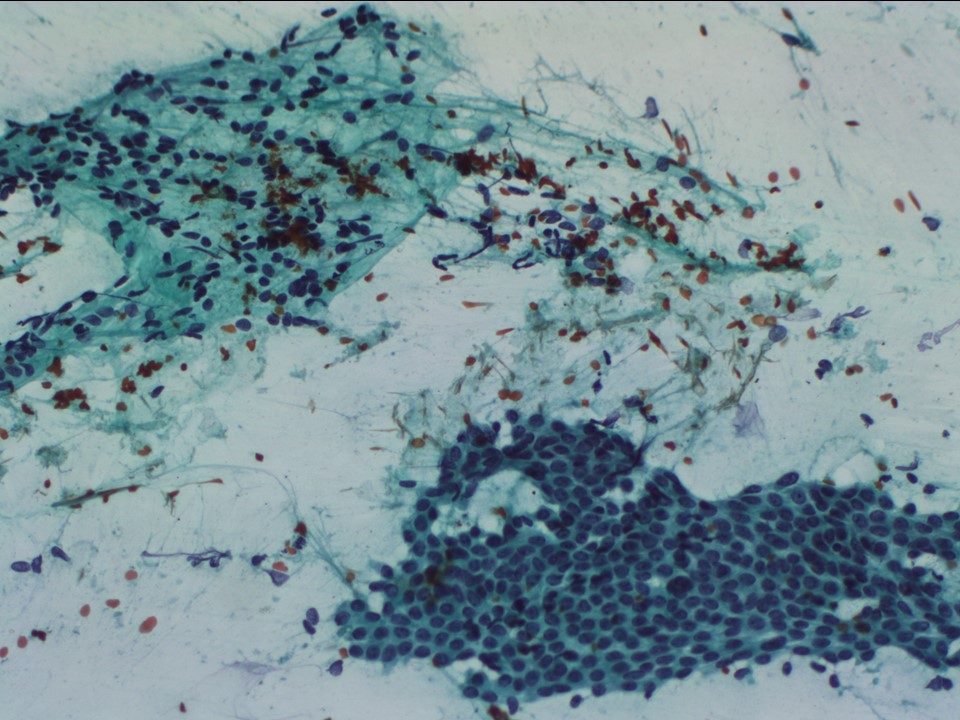
Further assessment advised: Referral for cytologyCytology:
| Cytology features: | |
| ‣ Type of sample: | FNAC |
| ‣ Site of biopsy: | |
| • Laterality: | Right |
| • Quadrant: | Central |
| • Localization technique: | Palpation |
| • Nature of aspirate: | Whitish |
| ‣ Cytological description: | Smears are very cellular and show loosely cohesive sheets of malignant ductal cells of low nuclear grade. Many single isolated malignant cells are seen. There are also many tightly cohesive sheets of benign ductal epithelial cells. A few sheets of benign apocrine ductal cells and foamy histiocytes are seen. |
| ‣ Reporting category: | Suspicious, probably in situ or invasive carcinoma |
| ‣ Diagnosis: | Suspicious, probably in situ or invasive carcinoma |
| ‣ Comments: | In view of mixture of malignant cells with many benign ductal cells and apocrine change, a core biopsy or frozen section is advisable to rule out invasive ductal carcinoma because DCIS and epithelial hyperplasia or proliferative fibrocystic change can have similar cytomorphology |
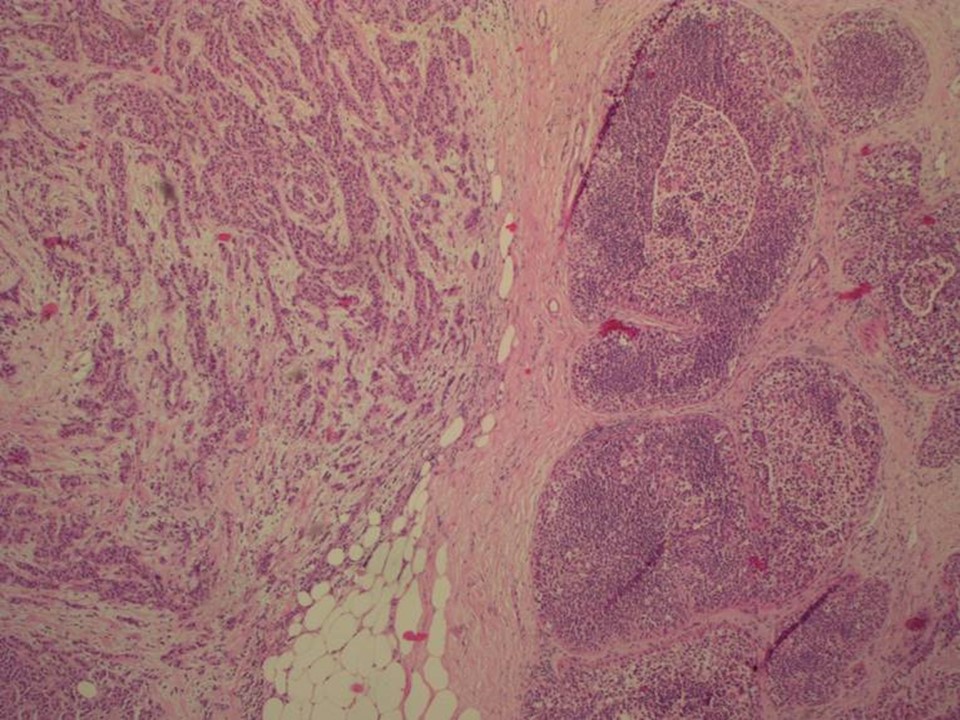
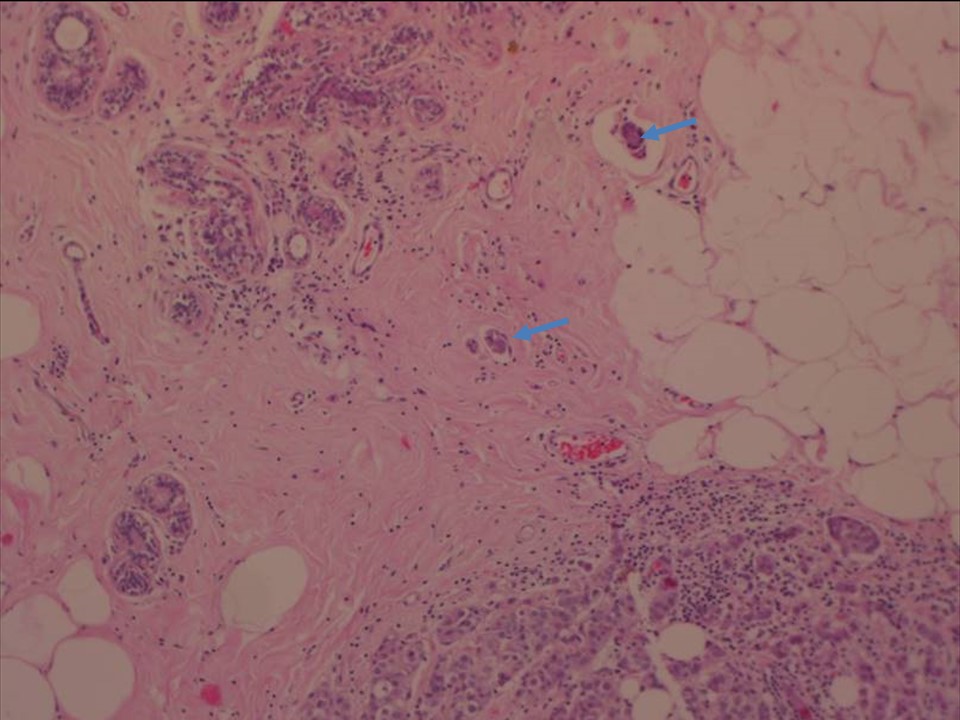
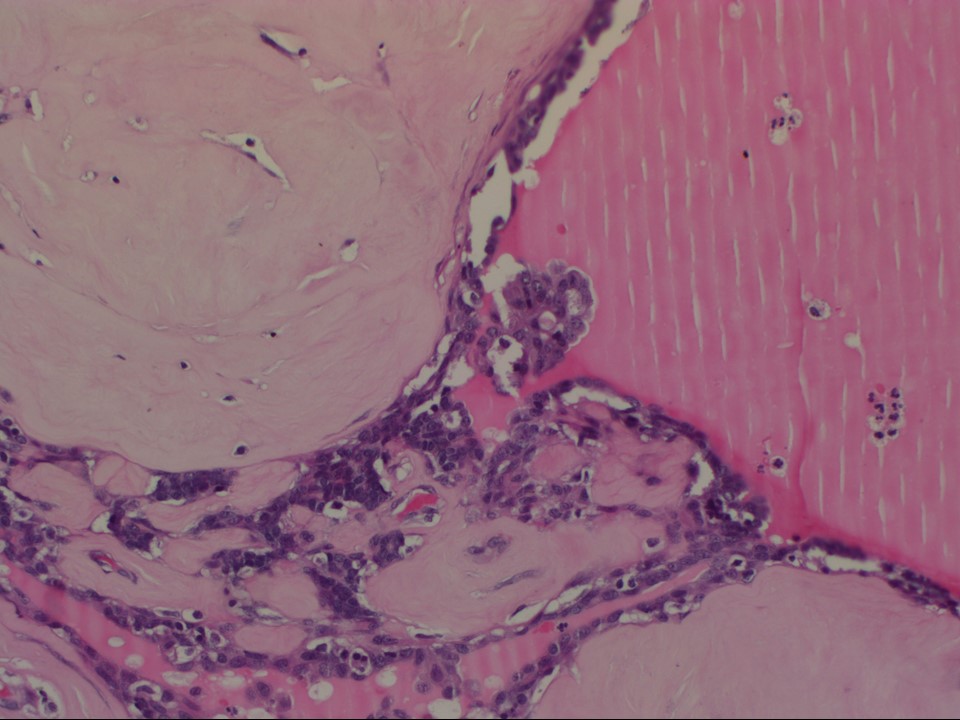
Histopathology:
MRM
| Histopathology features: | |
| ‣ Specimen type: | MRM |
| ‣ Laterality: | Right |
| ‣ Macroscopy: | Lumpectomy specimen (5.0 × 4.0 × 2.0 cm) with skin flap (2.0 × 0.7 cm), anteriorly. On serial sectioning, a firm whitish tumour (2.5 × 2.0 × 1.5 cm) with circumscribed margins was identified. Tumour is 1.7 cm from the skin and 1.8 cm from the base. |
| ‣ Histological type: | Invasive carcinoma of no special type |
| ‣ Histological grade: | Grade 2 (2 + 2 + 1 = 5) |
| ‣ Mitosis: | 7 |
| ‣ Maximum invasive tumour size: | 2.6 cm in greatest dimension |
| ‣ Lymph node status: | 0/19 |
| ‣ Peritumoural lymphovascular invasion: | Present |
| ‣ DCIS/EIC: | Present – papillary, solid, cribriform, comedo type |
| ‣ Margins: | Free of tumour |
| ‣ Pathological stage: | pT2N0 |
| ‣ Biomarkers: | |
| ‣ Comments: | Frozen section of the lumpectomy was done, reported as invasive carcinoma, followed by MRM. The adjacent breast shows fibrosis, apocrine metaplastic ducts, and multiple papilloma with hyalinized cores |
Case summary:
| Postmenopausal woman who underwent surgery for left breast cancer 4 years ago is on regular follow-up. Clinical examination of the right breast was found to be normal. Mammography and breast ultrasound dated 2017 reveal a new suspicious irregular mass lesion in the right breast. Compared with previous mammograms dated 2013 and 2014, follow-up mammogram reveals developing asymmetry in the right breast. Interval change is seen. Diagnosed as highly suggestive of malignancy, BI-RADS 5 on imaging, as suspicious for malignancy on cytology, and as invasive breast carcinoma of no special type, pT2N0 on histopathology. |
Learning points:
|