Home / Training / Manuals / Atlas of breast cancer early detection / Cases
Atlas of breast cancer early detection
Filter by language: English / Русский
Go back to the list of case studies
.png) Click on the pictures to magnify and display the legends
Click on the pictures to magnify and display the legends
BI-RADS Category (2018: Left BCS, post operative breast): 4C (high suspicion for malignancy)
| Case number: | 126 |
| Age: | 48 |
| Clinical presentation: | Premenopausal woman presented for mammography follow-up after breast-conserving surgery done 20 years ago for breast cancer. She had an increased risk of developing breast cancer because three other women in the family had been diagnosed with breast cancer. Clinical examination did not reveal any significant finding except the scar of previous surgery. |
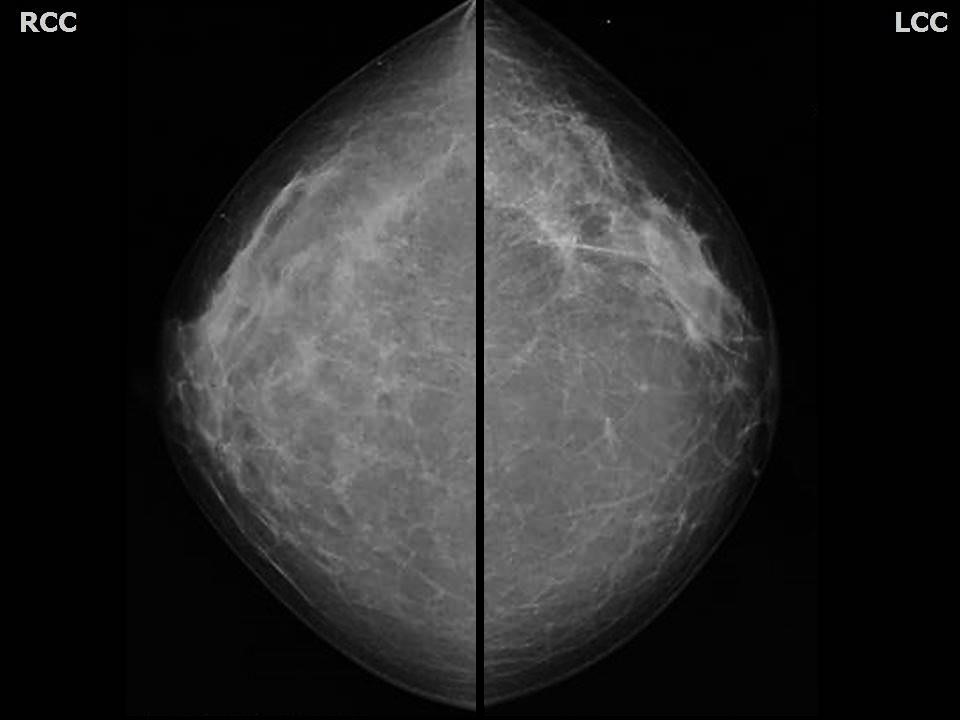
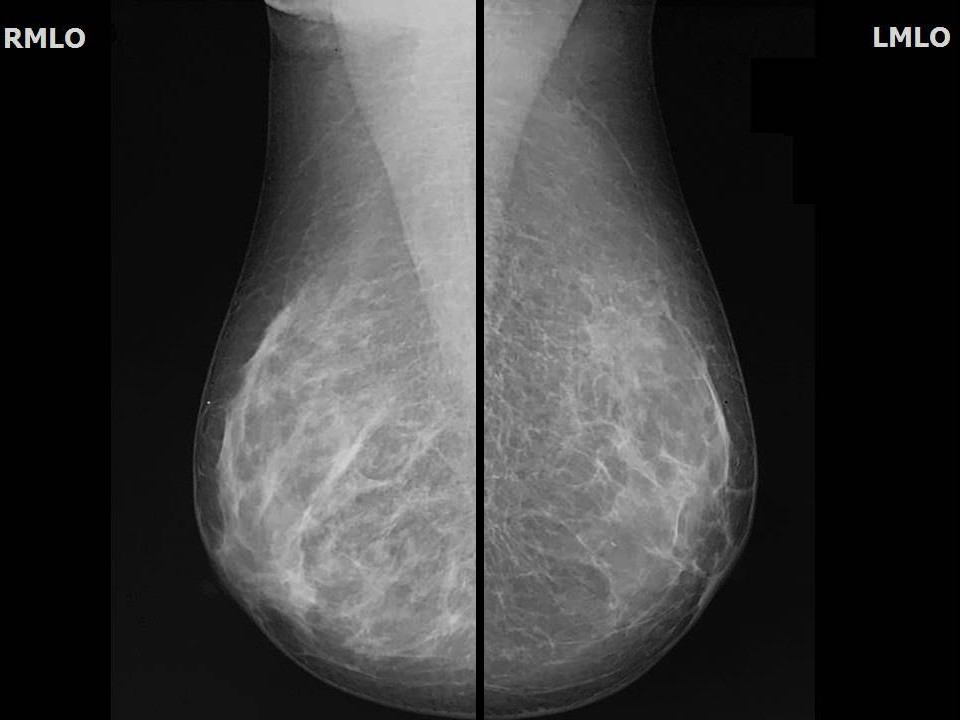
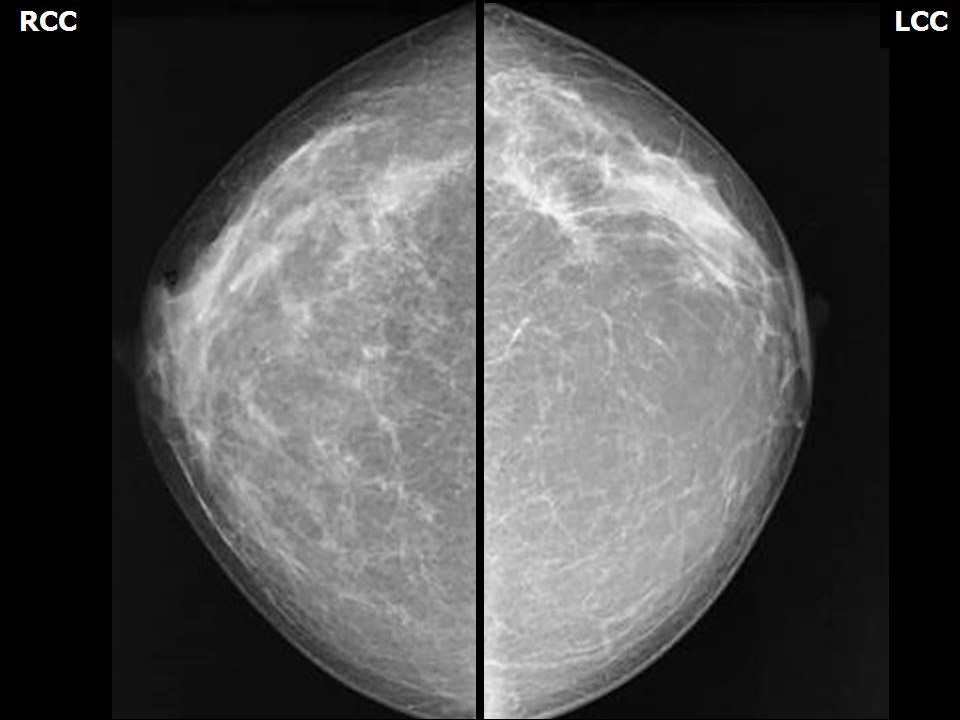
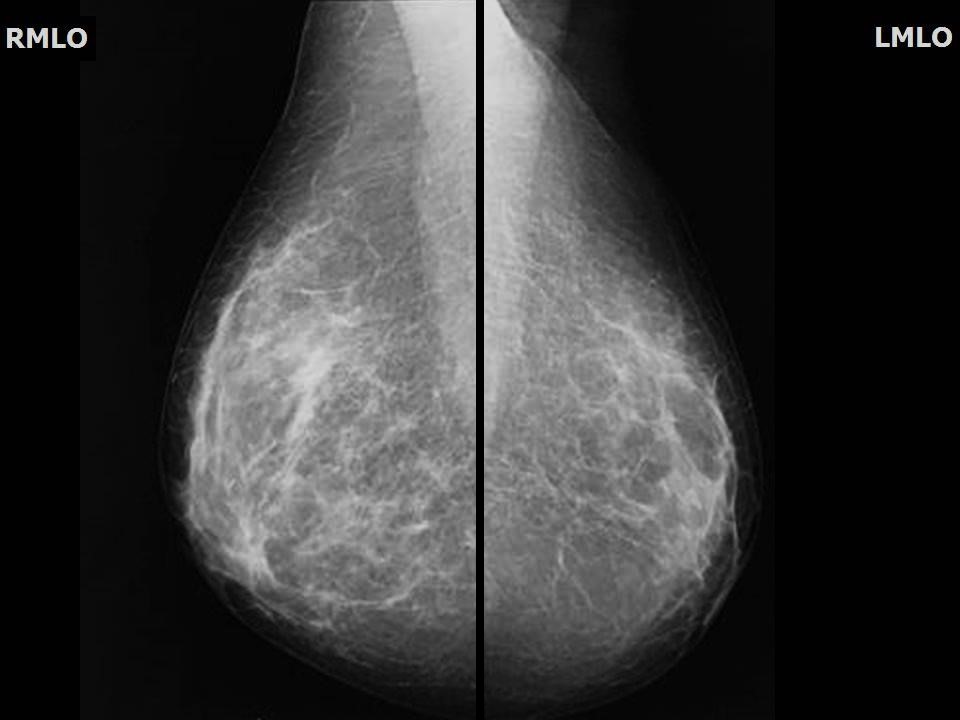
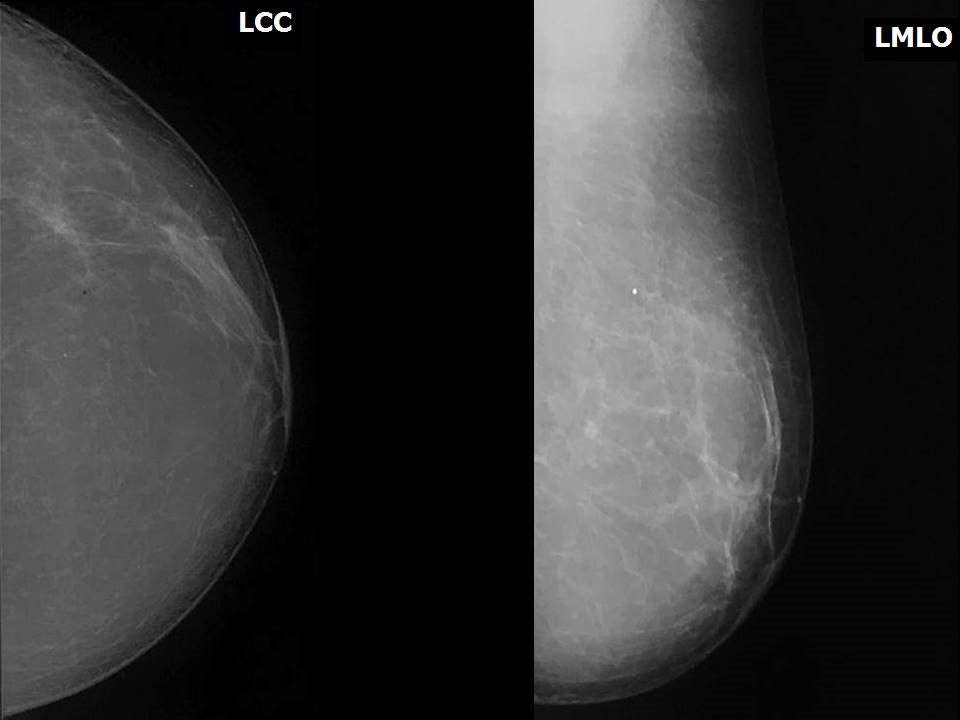
Mammography:
| Breast composition: | ACR category b (there are scattered areas of fibroglandular density) | Mammography features: |
| ‣ Location of the lesion: | Mammogram dated 2011, 2014, and 2016: Left breast (surgical scar at 2 o’clock) |
| ‣ Mass: | |
| • Number: | 0 |
| • Size: | None |
| • Shape: | None |
| • Margins: | None |
| • Density: | None |
| ‣ Calcifications: | |
| • Typically benign: | None |
| • Suspicious: | None |
| • Distribution: | None |
| ‣ Architectural distortion: | None |
| ‣ Asymmetry: | Present (surgical scar) |
| ‣ Intramammary node: | None |
| ‣ Skin lesion: | None |
| ‣ Solitary dilated duct: | None |
| ‣ Associated features: | None |
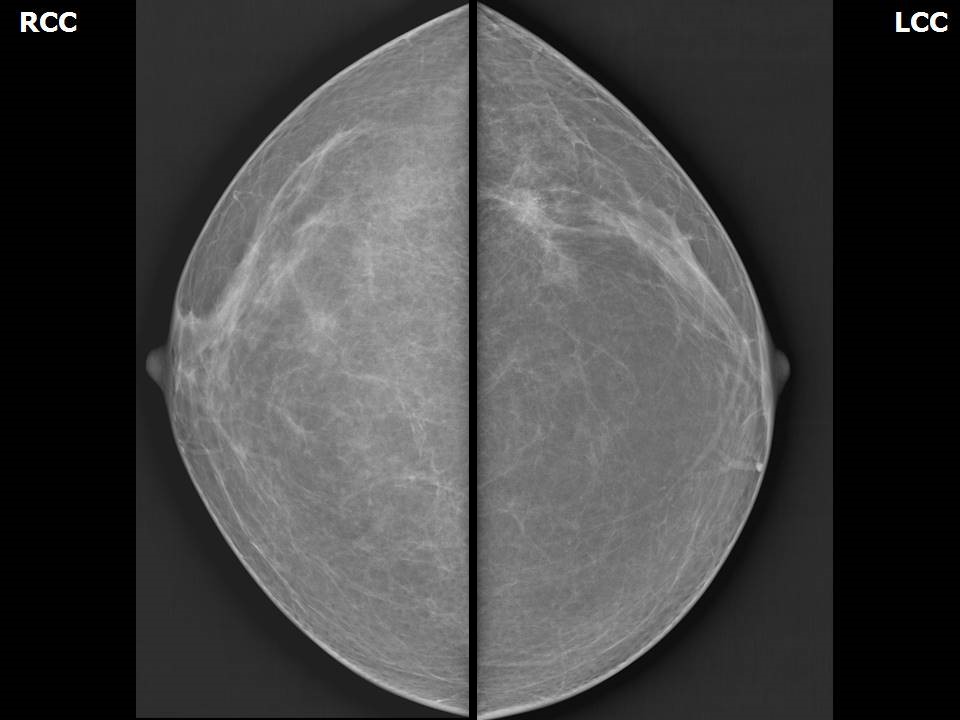
| Breast composition: | ACR category a (the breasts are almost entirely fatty) | Mammography features: |
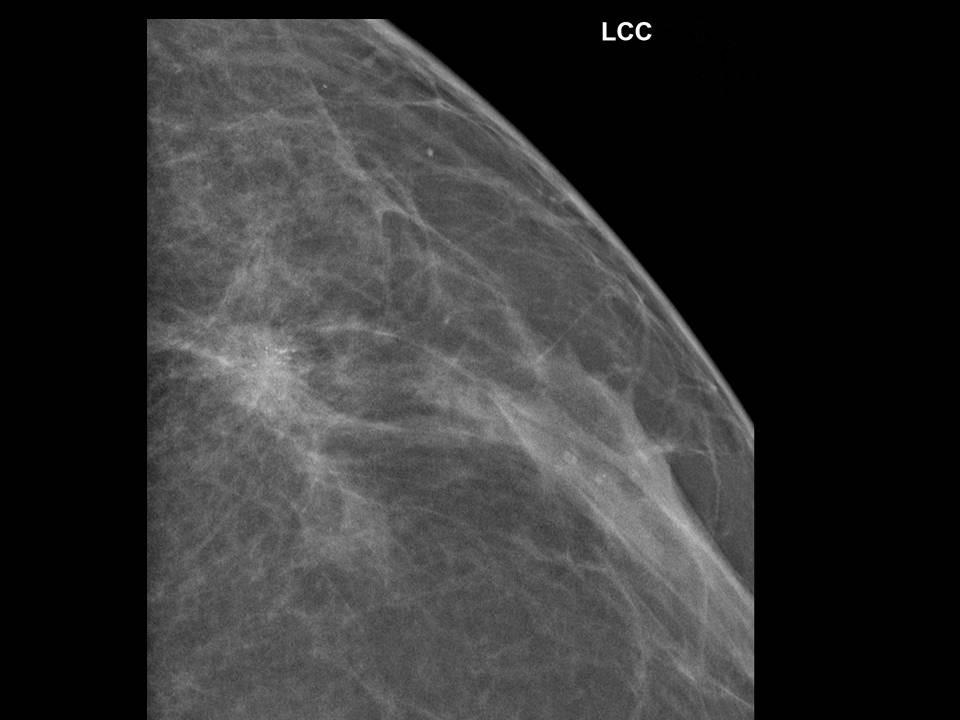
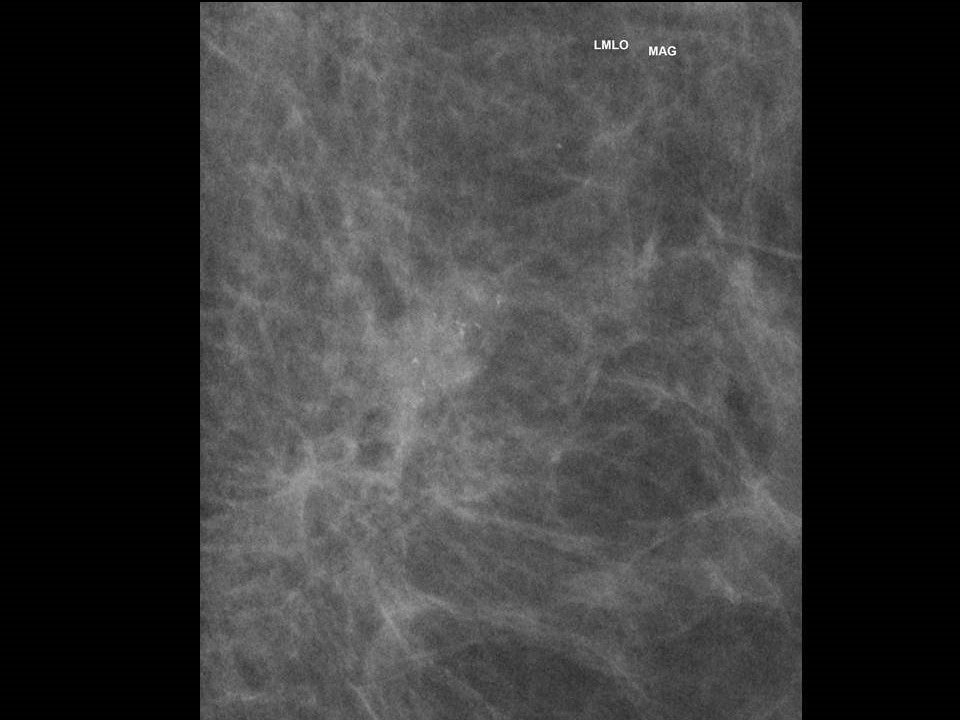
| ‣ Location of the lesion: | 2018: Left breast, upper outer quadrant at 2 o’clock, posterior third, along scar of earlier surgery |
| ‣ Mass: | |
| • Number: | 1 |
| • Size: | 1.3 × 0.6 cm (this is a new finding, developing asymmetry) |
| • Shape: | Irregular |
| • Margins: | Spiculated |
| • Density: | High |
| ‣ Calcifications: | |
| • Typically benign: | None |
| • Suspicious: | Fine pleomorphic |
| • Distribution: | Grouped |
| ‣ Architectural distortion: | Focal (post-breast-conserving surgery scar) |
| ‣ Asymmetry: | Focal |
| ‣ Intramammary node: | None |
| ‣ Skin lesion: | None |
| ‣ Solitary dilated duct: | None |
| ‣ Associated features: | Calcifications – fine pleomorphic |
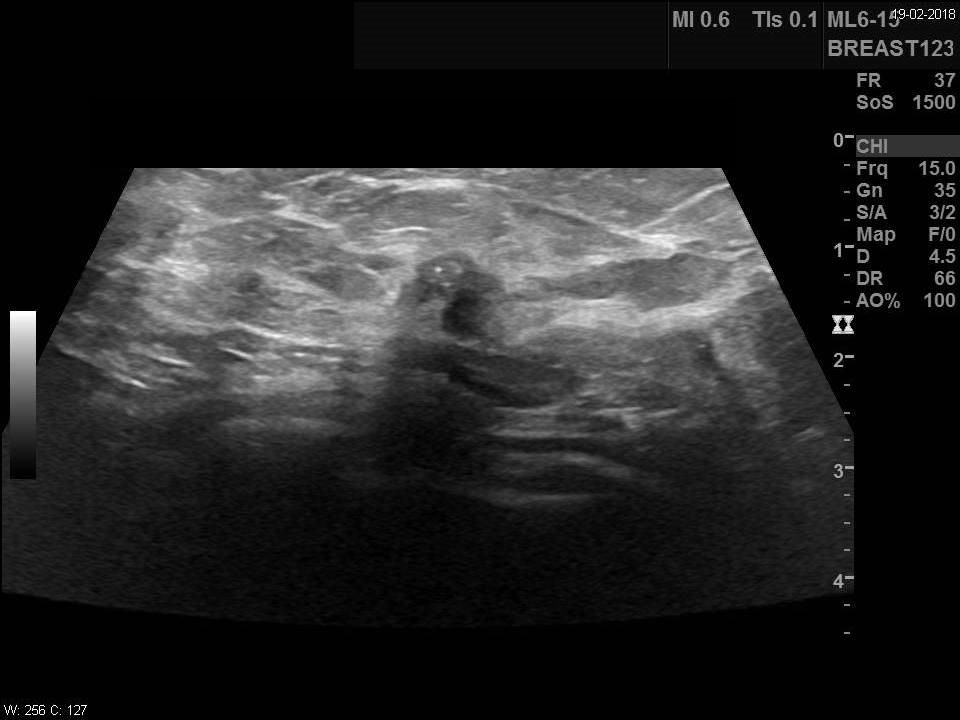
Ultrasound:
| Ultrasound features: 2018: Left breast, outer quadrant at 2 o’clock, along scar of earlier surgery | |
| ‣ Mass | |
| • Location: | 2018: Left breast, outer quadrant at 2 o’clock, along scar of earlier surgery |
| • Number: | 1 |
| • Size: | 0.8 × 0.7 cm (this is a new finding, developing asymmetry) |
| • Shape: | Irregular |
| • Orientation: | Not parallel |
| • Margins: | Irregular |
| • Echo pattern: | Hypoechoic |
| • Posterior features: | No posterior features |
| ‣ Calcifications: | Present in mass |
| ‣ Associated features: | Architectural distortion |
| ‣ Special cases: | None |
BI-RADS:
BI-RADS Category (2011, 2014, 2016: Left BCS, post operative breast): 2 (benign)BI-RADS Category (2018: Left BCS, post operative breast): 4C (high suspicion for malignancy)
Further assessment:
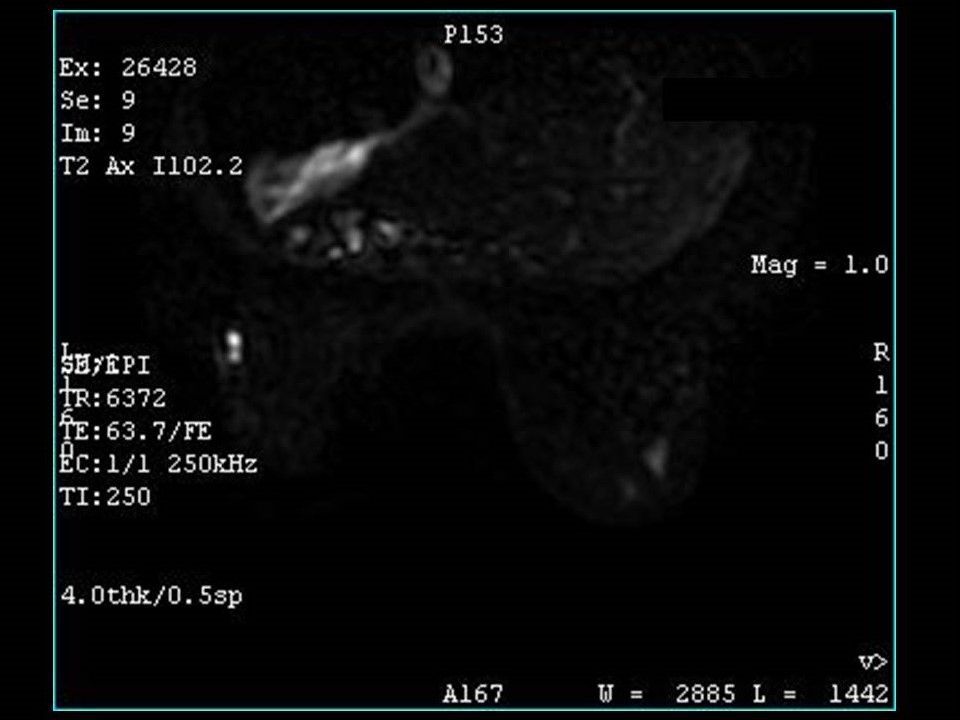
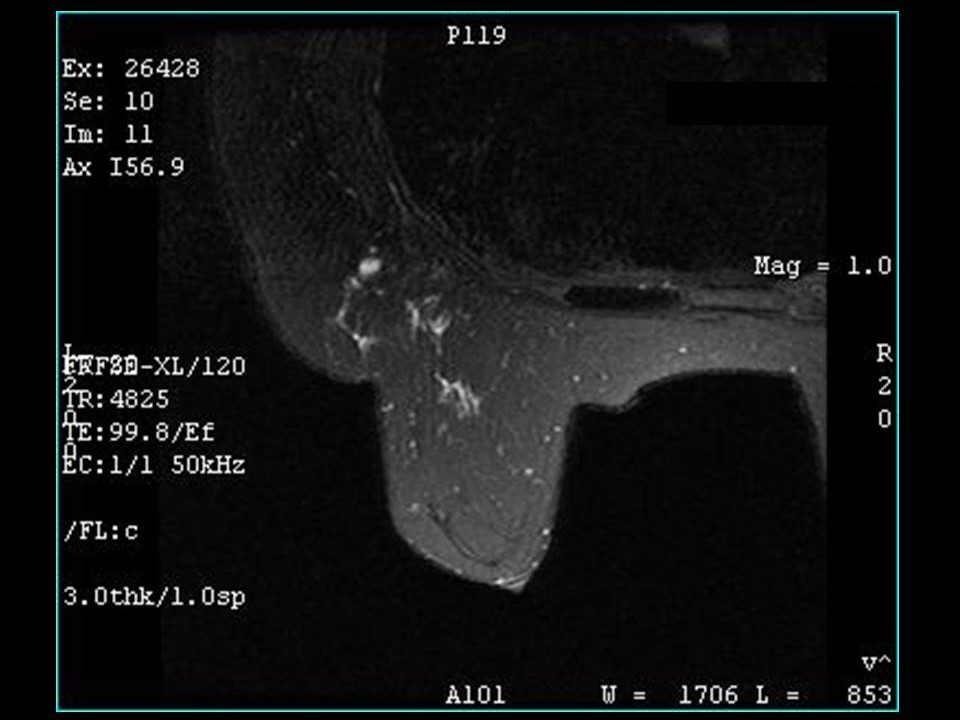
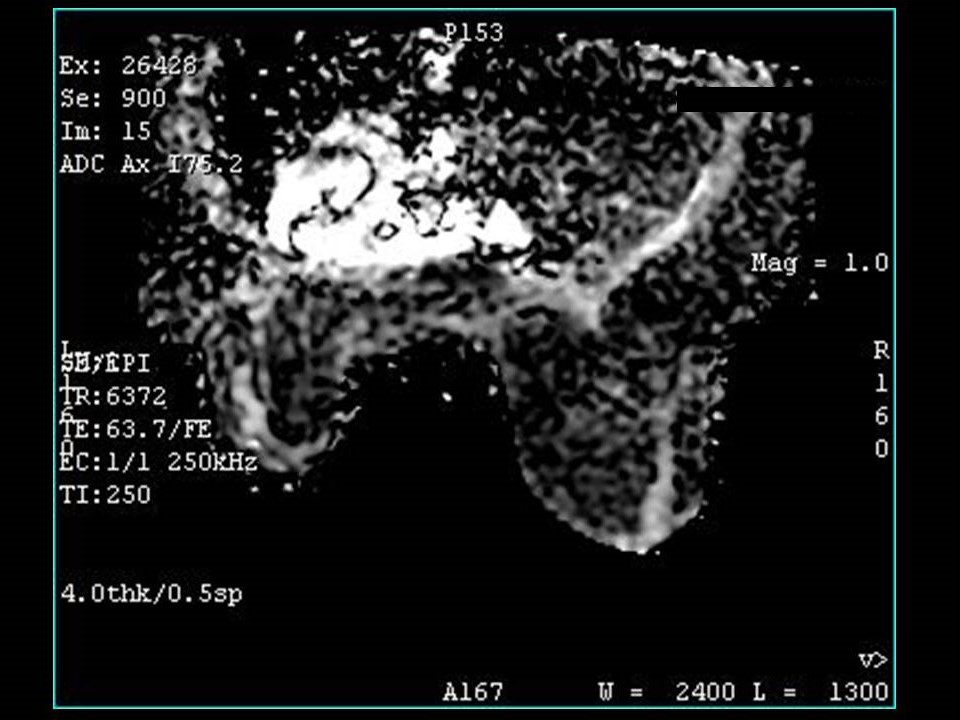
Further assessment advised: Referral for core biopsy and further imaging with breast MRIMRI:
| MRI features: | ||
| ‣ MRI features: | Amount of fibroglandular tissue: ACR category a (the breasts are almost entirely fatty). Background parenchymal enhancement: Minimal (< 25%), symmetrical | |
| ‣ Location: | Left breast, inferolateral quadrant at 2 o’clock | |
| ‣ Focus: | No | |
| ‣ Mass: | ||
| • Shape: | No | |
| • Margin: | No | |
| • Internal enhancement: | No | |
| • Kinetic curve: | Type 2 | |
| ‣ Non-mass enhancement: | ||
| • Distribution: | Central portion of left breast at 2 o’clock | |
| • Internal enhancement: | Heterogeneous, predominantly peripheral | |
| ‣ Non-enhancing findings: | No | |
| ‣ Associated features: | Postoperative scar | |
| ‣ Axillary nodes: | Left axillary lymph node (0.8 × 0.7 cm) in axillary tail | |
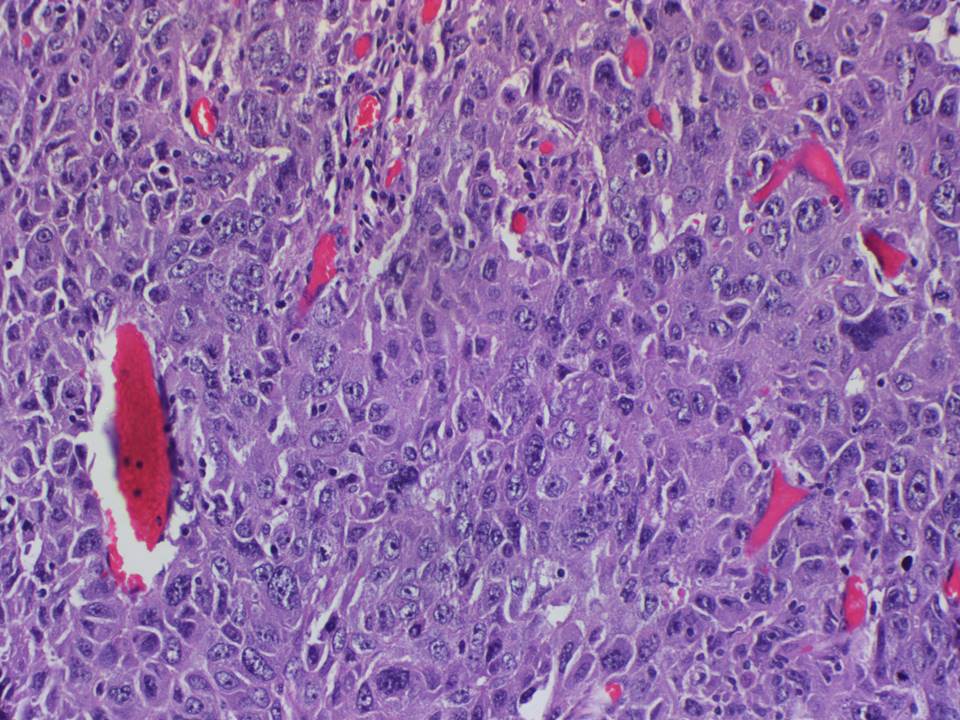
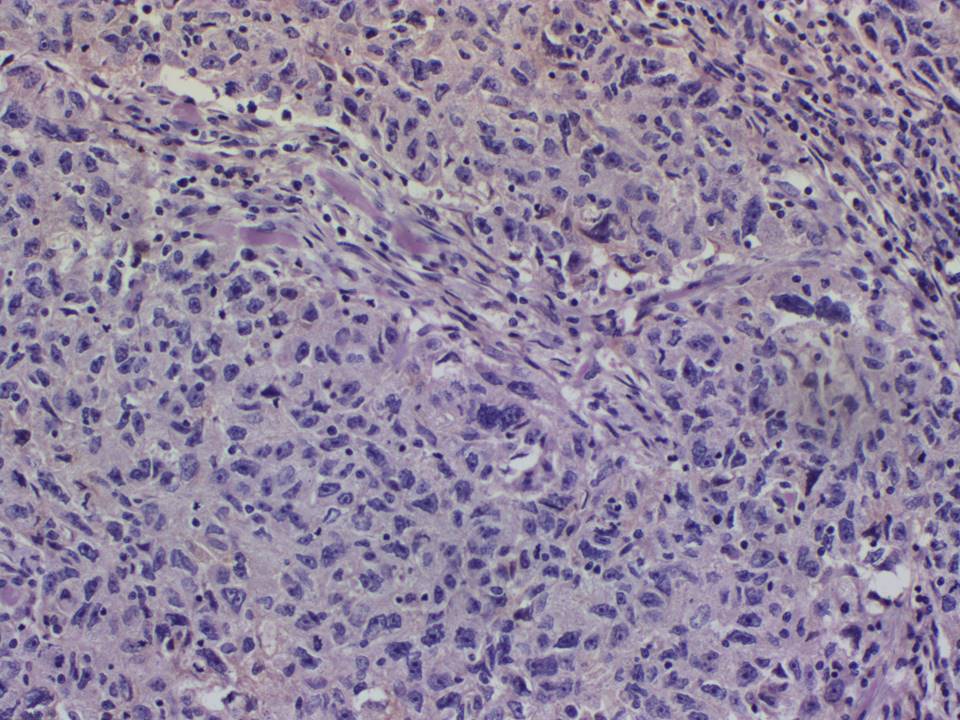
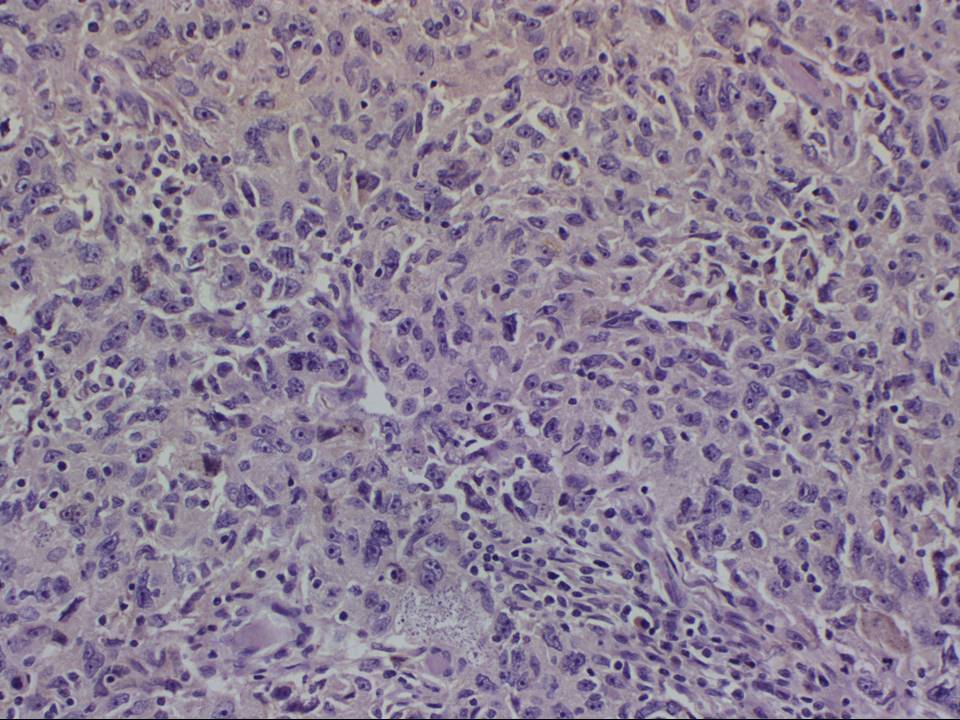
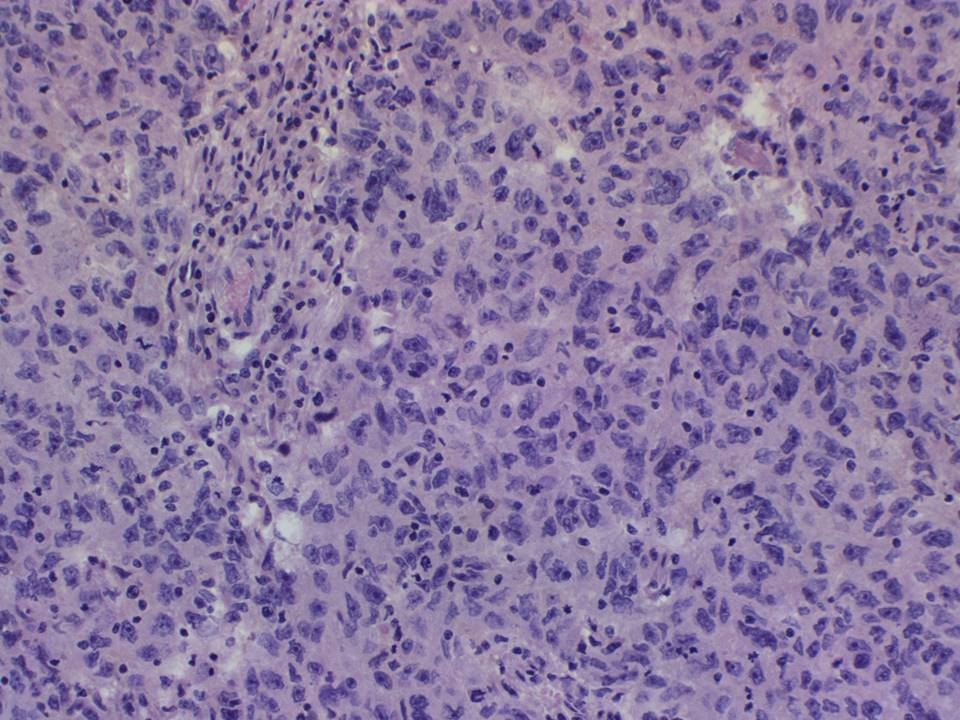
Histopathology:
Left breast, incisional biopsy
| Histopathology features: | |
| ‣ Specimen type: | Left breast, incisional biopsy |
| ‣ Laterality: | |
| ‣ Macroscopy: | Two soft tissue bits (2.1 × 1.5 × 1.0 cm and 2.3 × 1.6 × 1.0 cm) |
| ‣ Histological type: | Invasive breast carcinoma of no special type |
| ‣ Histological grade: | Grade 3 (3 + 3 + 2 = 8) |
| ‣ Mitosis: | |
| ‣ Maximum invasive tumour size: | |
| ‣ Lymph node status: | |
| ‣ Peritumoural lymphovascular invasion: | |
| ‣ DCIS/EIC: | |
| ‣ Margins: | |
| ‣ Pathological stage: | |
| ‣ Biomarkers: | ER negative, PR negative, and HER2 negative (triple negative) |
| ‣ Comments: | Desmoplasia and calcification noted |
Case summary:
| Premenopausal woman, operated for left breast cancer 20 years ago, in 1998, presented for follow-up. She has increased risk of developing breast cancer because three other women in the family had been diagnosed with breast cancer. Previous serial 18 years follow-up mammogram images up to 2016 are available for comparison. Mammography and breast ultrasound dated 2018 reveal a new suspicious irregular lesion in the left breast with pleomorphic microcalcifications within. Compared with the previous mammogram, dated 2016, follow-up reveals developing asymmetry in the left breast. Interval change is seen, diagnosed as highly suspicious of malignancy, BI-RADS category 4C on imaging, and invasive breast carcinoma, NST on core biopsy. |
Learning points:
|