Chapters
Introduction
Visual inspection after application of acetic acid (VIA)
Determining eligibility for ablative treatment after application of acetic acid
Anatomical considerations
Cervical epithelium
Physiological changes of cervical epithelium
Neoplastic changes of the cervical epithelium
Changes in the cervical epithelium after application of acetic acid
Instruments, consumables, and setup required for examination after application of acetic acid
VIA procedure
Interpretation of VIA test results
Preventing errors in VIA
Management of women with an abnormal VIA test
Steps to determine eligibility for ablative treatment
Role of Lugolís iodine in identifying the transformation zone for treatment
Treatment by cryotherapy
Treatment by thermal ablation
Videos
Preparation of Monselís solution
Infection prevention
Case study
Quiz
Acknowledgement
Suggested citation
Copyright
Home / Training / Manuals / Atlas of visual inspection of the cervix with acetic acid for screening, triage, and assessment for treatment
.png)
Click on the pictures to magnify and display the legends
Atlas of visual inspection of the cervix with acetic acid for screening, triage, and assessment for treatment
Filter by language: English / FranÁais / EspaŮol / Русский / українськаManagement of women with an abnormal VIA test |
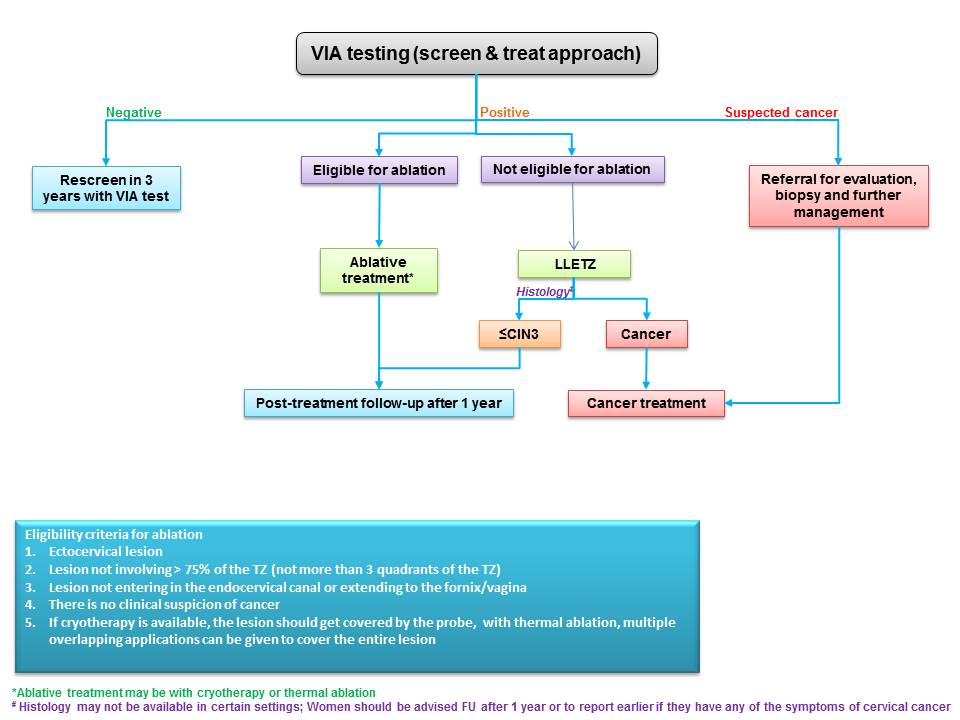
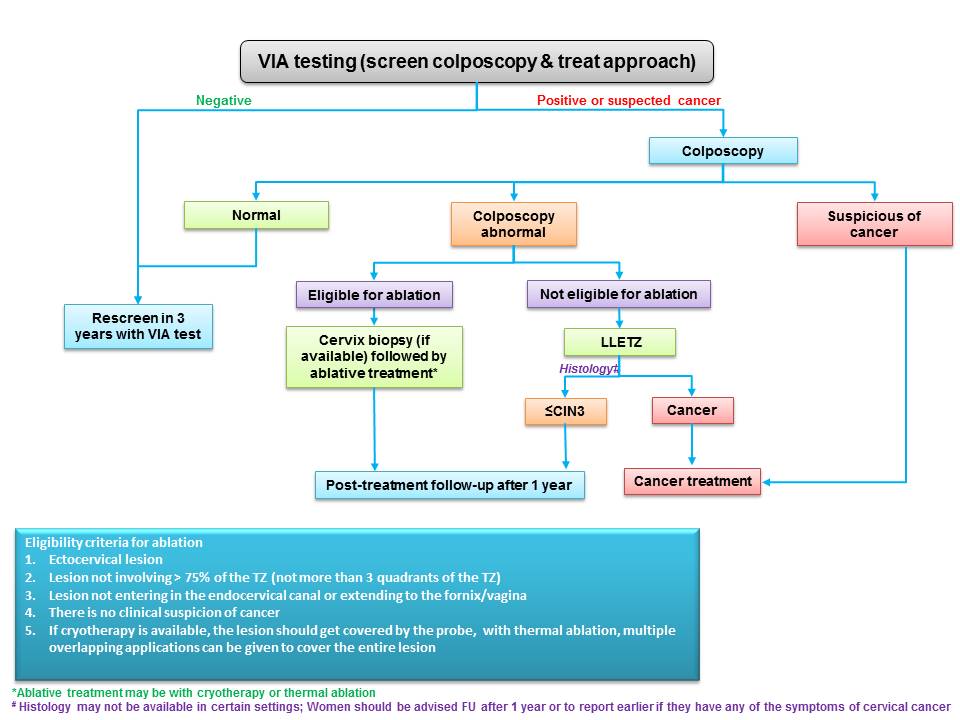
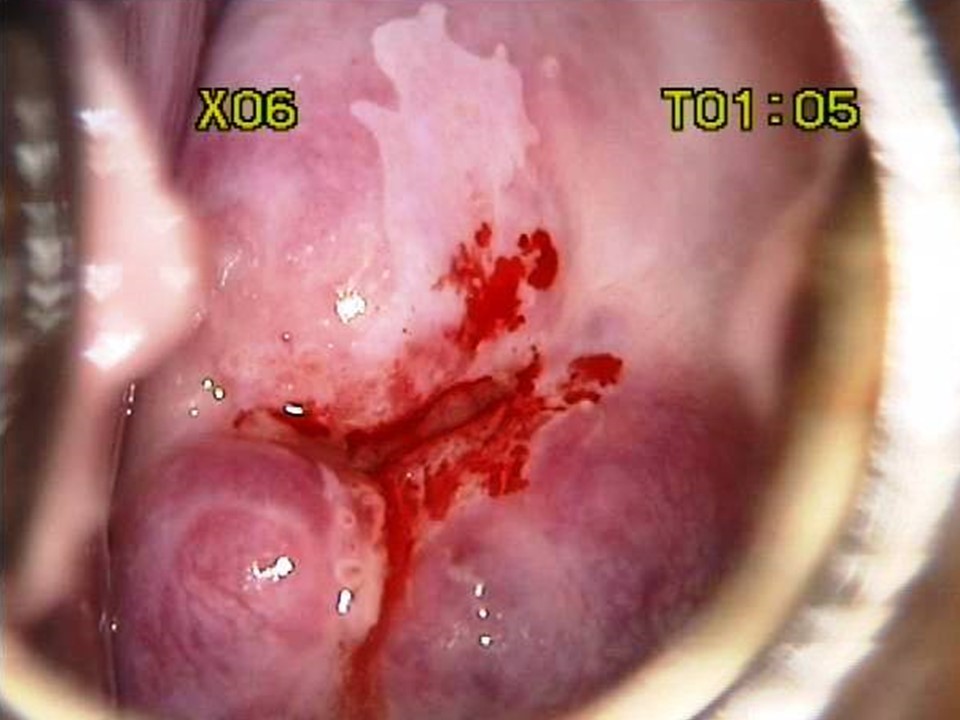
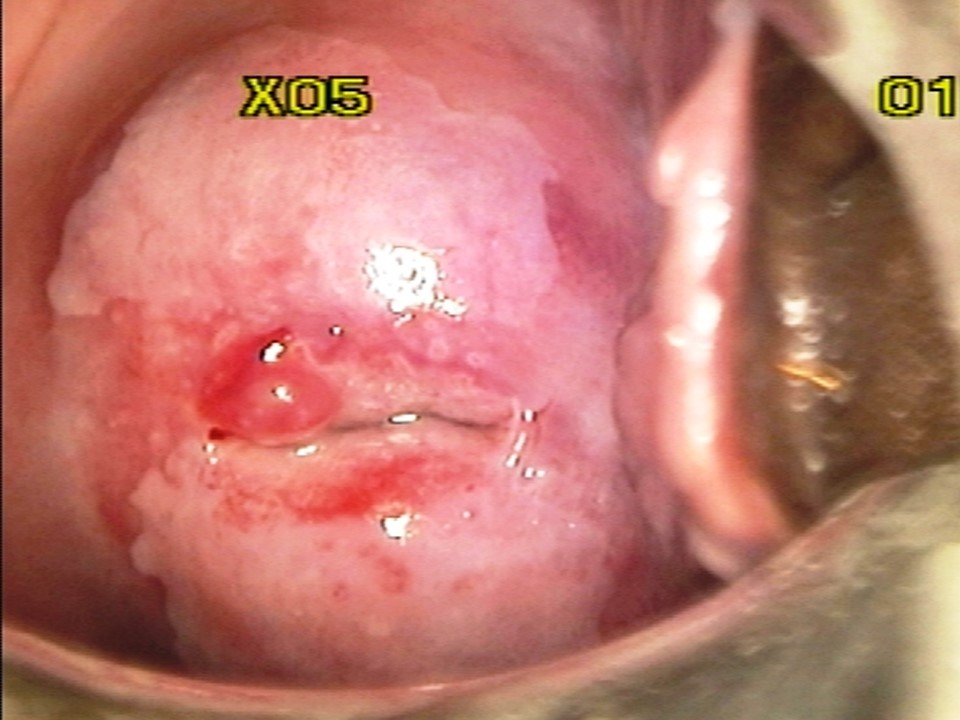
Women who test negative on VIA are to be advised to undergo repeat screening, depending on the recommended upper age and screening frequency of the country or programme. WHO recommends screening of women every 3 years when using VIA. WHO also recommends that priority should be given to screening women aged 30Ė49 years in the general population of women (25-49 years in HIV positive women). Screening may be extended to women aged 50-65 years. However, adequate facilities to perform excisional treatment should be made available as majority of the post-menopausal women will not be eligible for ablation, if tested positive. The success of cervical cancer screening depends on appropriate management of screen-positive women. Because VIA positivity by itself does not indicate the presence of cervical premalignant or malignant lesions, a confirmatory test is needed in ideal circumstances. The confirmatory test may be colposcopy. The colposcope enables examination of the cervix under a good light source and with different levels of magnification. Depending on the outcomes of colposcopic examination, a colposcopist may decide to either take a biopsy from the abnormal area or proceed directly to treatment. The VIA-positive women with a normal colposcopy result are reassured and advised to attend repeat screening as per protocol. To learn more about colposcopy, access the Atlas of Colposcopy: Principles and Practice. In many resource-limited settings colposcopy and histopathology services have limited availability. The World Health Organization recommends for such settings a more realistic approach of offering treatment to as many VIA-positive women as feasible during the same screening visit. This is known as the screen-and-treat approach, in which treatment is offered to screen-positive women directly without verification of disease by colposcopy or histopathology. The screen-and-treat approach has the potential to improve the efficiency of a screening programme, because it increases compliance of screen-positive women with treatment and reduces referral for colposcopy. Screen and treat approach VIA has the advantage of being a point-of-care screening test, because it provides the test results immediately and enables treatment decisions to be made during the same visit as screening. VIA simultaneously enables assessment of suitability for ablative treatment based on the location of the squamocolumnar junction, the size and extent of the lesion, and abnormal features (whether suggestive of invasive cancer). Thus, at the end of the VIA examination the provider should not only give a diagnosis (VIA-negative, VIA-positive, or suspicious of invasive cancer) but also suggest the most appropriate management for the VIA-positive women that may be either of the following:
Management of HPV positive women depending on VIA triage outcomes Similar principles of management apply when VIA is used to triage HPV positive women. HPV positive women with a negative VIA test need to be recalled after two years for the repeat HPV test (preferred) (and after one year if living with HIV) or repeat VIA. HPV positive women with suspected cancer on VIA are to be appropriately referred for further assessment and biopsy. The VIA positive women are assessed for suitability of ablative treatment and treated with either cryotherapy or thermal ablation at the same sitting. VIA positive women ineligible for ablation are to be offered excisional treatment, either at the same clinic or at an appropriate center. Treatment of cervical premalignant lesions Cervical premalignant lesions may be treated by either ablative or excisional techniques. Ablative techniques use either cold injury (cryotherapy) or heat injury (thermal ablation) to destroy the abnormal epithelium of the transformation zone of the cervix. The most widely used excisional technique is large loop excision of the transformation zone (LLETZ), also known as the loop electrosurgical excision procedure (LEEP). The entire TZ is removed using a loop made of metallic wire and powered by an electrosurgical unit to treat the cervical precancer. The TZ may be excised with a surgical knife and the procedure is known as cold knife conization (CKC). Alternatively, a needle or a straight wire powered by an electrosurgical unit may also be used to excise the TZ. The procedure is known as NETZ or SWETZ. Whereas excisional techniques can be used to treat all cervical premalignant lesions, ablative techniques are suitable only for lesions that fulfil certain selection criteria, as described below. Ablative techniques are simpler and have fewer complications compared with excisional techniques. We will describe in detail the procedure of ablative treatment in the next sections. To learn more about LLETZ and CKC, please click on the following link. In a screen-and-treat setting, every VIA-positive woman is to be assessed for suitability of the lesion for ablative treatment, irrespective of whether VIA is the screening test or a test to triage HPV positive women. Following are the criteria to select a VIA-positive woman for ablative treatment:
There is an additional criterion, if cryotherapy is the technique used for ablative therapy. The cryotherapy probe should be able to cover the transformation zone. This is not a requirement for thermal ablation, because the probe for thermal ablation can be applied to the cervix multiple times.
If histopathology facilities are available, a punch biopsy should be obtained from the abnormal lesion before performing ablative treatment. The entire specimen removed at excisional treatment requires histopathological evaluation to determine whether the precancer has been completely removed and to exclude any focus of invasive cancer.
|
Click on the pictures to magnify and display the legends
IARC, 150 Cours Albert Thomas, 69372 Lyon CEDEX 08, France - Tel: +33 (0)4 72 73 84 85 - Fax: +33 (0)4 72 73 85 75
© IARC 2026 - All Rights Reserved.
© IARC 2026 - All Rights Reserved.