Chapters
Introduction
Visual inspection after application of acetic acid (VIA)
Determining eligibility for ablative treatment after application of acetic acid
Anatomical considerations
Cervical epithelium
Physiological changes of cervical epithelium
Neoplastic changes of the cervical epithelium
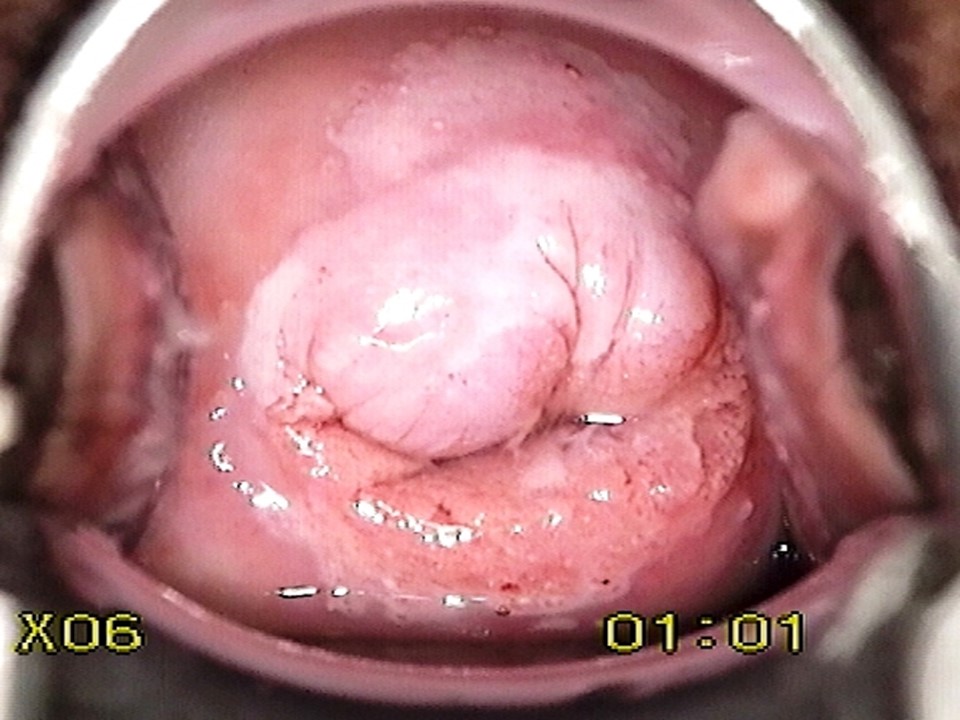
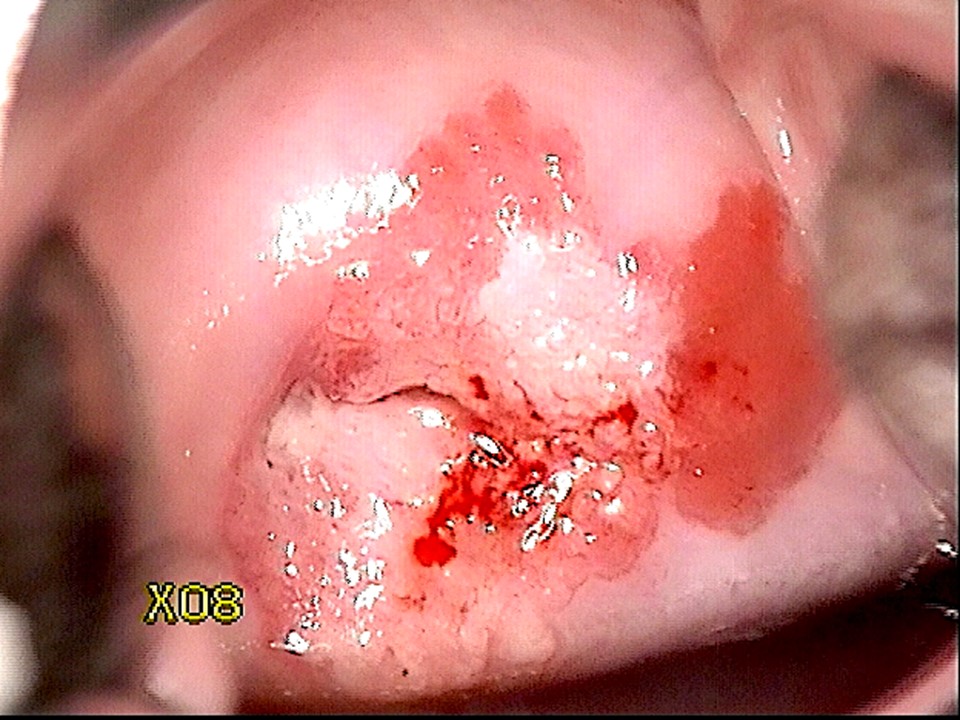
Changes in the cervical epithelium after application of acetic acid
Instruments, consumables, and setup required for examination after application of acetic acid
VIA procedure
Interpretation of VIA test results
Preventing errors in VIA
Management of women with an abnormal VIA test
Steps to determine eligibility for ablative treatment
Role of Lugolís iodine in identifying the transformation zone for treatment
Treatment by cryotherapy
Treatment by thermal ablation
Videos
Preparation of Monselís solution
Infection prevention
Case study
Quiz
Acknowledgement
Suggested citation
Copyright
Home / Training / Manuals / Atlas of visual inspection of the cervix with acetic acid for screening, triage, and assessment for treatment
.png)
Click on the pictures to magnify and display the legends
Atlas of visual inspection of the cervix with acetic acid for screening, triage, and assessment for treatment
Filter by language: English / FranÁais / EspaŮol / Русский / українськаNeoplastic changes of the cervical epithelium Ė Genesis of cervical cancer |
The natural history of cervical cancer spans over a few years to decades, starting with infection with human papillomavirus (HPV). There are about 14 types of HPV that can cause cervical cancer and few other cancers (vulvar and vaginal cancers in females, penile cancer in males, anal and oropharyngeal cancers in both sexes); these are called high-risk or oncogenic HPV types. Out of these, HPV 16 and 18 are the most oncogenic. Two HPV types (HPV 6 and 11) are responsible for nearly 90% of the genital warts. HPV is a very common sexually transmitted infection. Most women clear the infection as they develop natural immunity against the virus. However, a small proportion of women infected with high-risk HPV cannot clear the infection. The women with persistent infection are at high risk of developing cervical cancer and also other genital cancers and anal cancer. The persistence of infection first leads to the development of a premalignant condition of cervix, known as cervical intraepithelial neoplasia (CIN). A similar premalignant lesion that develops over the columnar epithelium is known as adenocarcinoma in situ (AIS). If it remains undetected and is left untreated, CIN or AIS may lead to invasive cervical cancer after 5 Ė10 years.
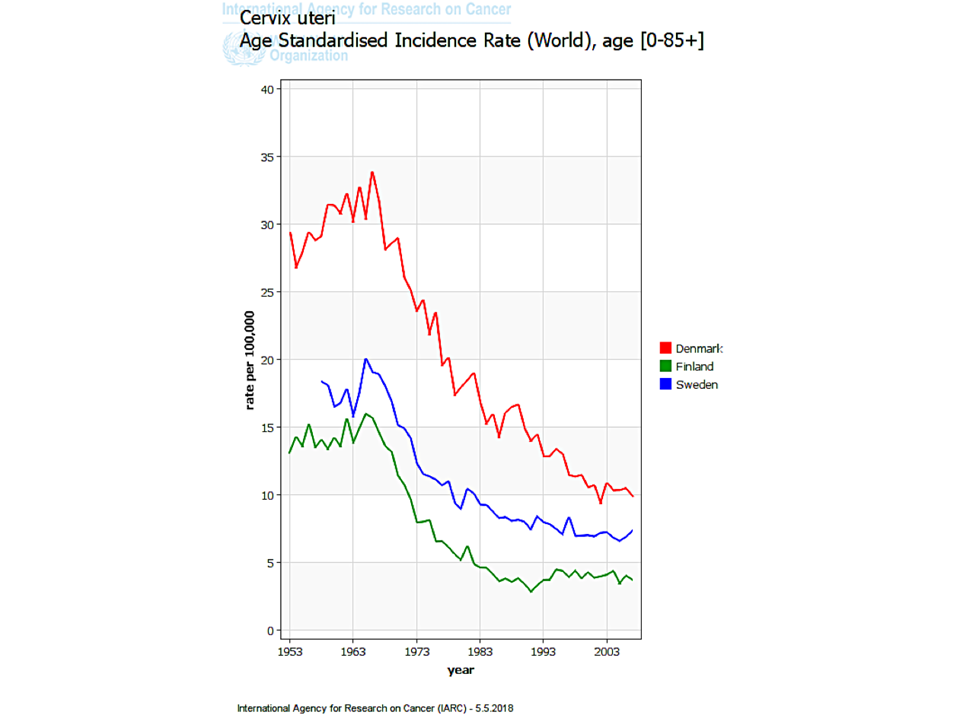
Cervical cancer is predominantly of two types: squamous cell cancer (which arises from the squamous epithelium) and adenocarcinoma (which arises from the columnar epithelium). Each type of cancer is preceded by the occurrence of a precancerous change of the epithelium. The precursor of squamous cell cancer is known as cervical intraepithelial neoplasia (CIN), and that of adenocarcinoma is known as adenocarcinoma in situ (AIS). Squamous cell cancers are the most common, accounting for 80Ė90% of all cervical cancers. Hence, CIN is much more common than AIS. Cervical cancer has a slow natural history. Women with CIN or AIS do not have any symptoms. There are appropriate tests that, when administered routinely to women after a certain age, are capable of detecting the precancers. Treatment of precancers may cure about 90% of them, and successfully treated women are prevented from developing cervical cancer in the future. This is the basic principle of cervical cancer screening. Regular screening of women with an appropriate test starting at 25 or 30 years of age, followed by treatment of the CIN or AIS lesions detected through screening, can significantly reduce the incidence of cervical cancer in the population. In countries with well-organized screening programmes, in which women are systematically invited to undergo a screening test at an interval of 3Ė5 years, there have been drastic reductions in both the incidence of cervical cancer and mortality from the disease. The most commonly used cervical cancer screening tests are the Pap smear (cytology), VIA, and HPV detection tests.
The next section provides more information about cervical intraepithelial neoplasia (CIN). |
Click on the pictures to magnify and display the legends
IARC, 150 Cours Albert Thomas, 69372 Lyon CEDEX 08, France - Tel: +33 (0)4 72 73 84 85 - Fax: +33 (0)4 72 73 85 75
© IARC 2025 - All Rights Reserved.
© IARC 2025 - All Rights Reserved.