Learning colposcopy
Colposcopic appearance of normal cervix
The colposcopic examination
Detection of infections & benign conditions of cervix
Detection of cervical neoplasias
Treatment of cervical intraepithelial neoplasia
Treatment by cryotherapy
Treatment by thermal ablation
Treatment by LLETZ (LEEP)
Treatment by cold-knife conization (CKC)
Cases
Normal
Squamous metaplasia and ectropion
Inflammation and cervicitis
Low grade
High grade
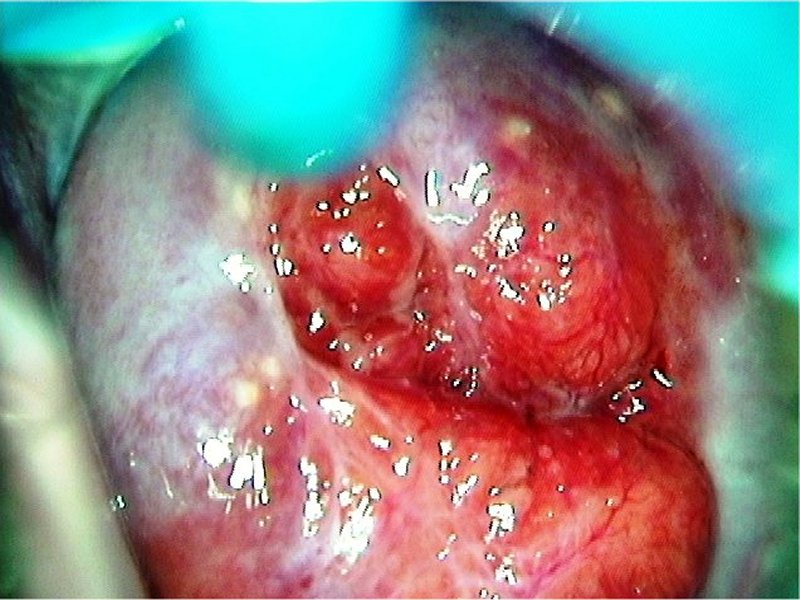
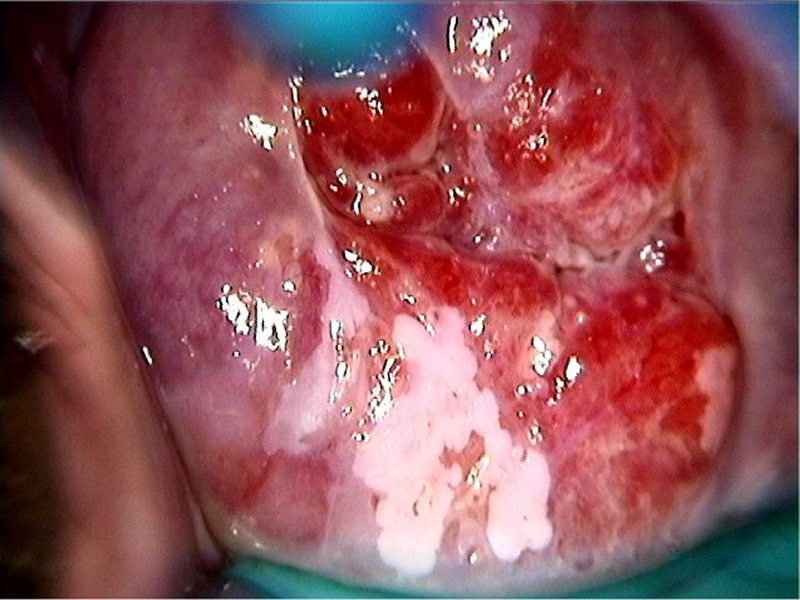
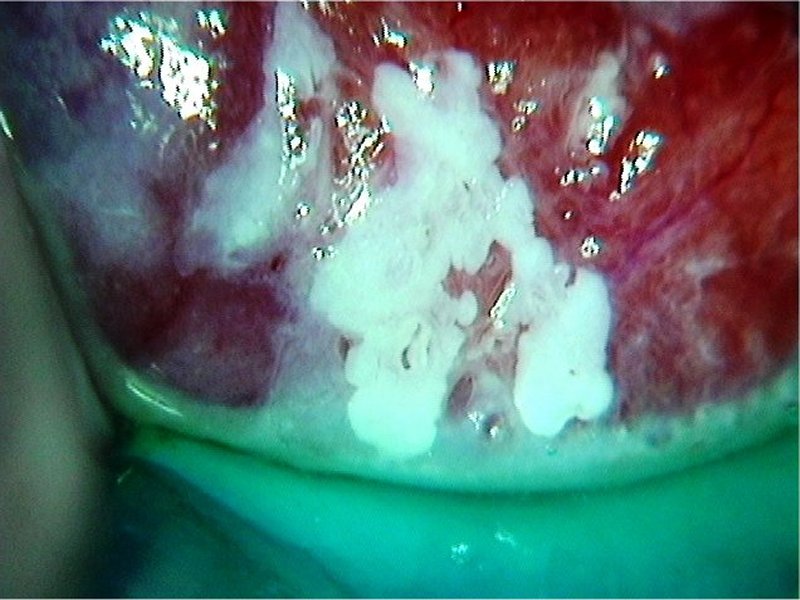
Early and advanced cancers
Miscellaneous
Post treatment
Search with IFCPC criteria
Search with Swede score criteria
Quiz Foreword
Acknowledgement
Authors
Suggested citation