Introduction
Different approaches to screening and treatment of cervical precancer
Anatomical considerations
Physiological changes of the cervical epithelium
Neoplastic changes of the cervical epithelium
HPV tests – Variation between tests
Instruments, consumables, and setup required
Procedure to collect samples for HPV testing
Interpretation of HPV test results
Management of women with a positive HPV test result
Treatment of cervical intraepithelial neoplasia – principles
Steps to determine eligibility for ablative treatment
Role of Lugol’s iodine in identifying the transformation zone for treatment
Treatment by cryotherapy
Treatment by thermal ablation
Using an HPV test as the test of cure in women treated for cervical abnormalities or cervical intraepithelial neoplasia (CIN)
Infection prevention
Case studies
VIA triage outcome (applicable in screen-and-treat setting only) – negative cases
VIA triage outcome – positive cases
VIA triage outcome – suspicious of cancer cases
Foreword
Acknowledgement
Authors
Suggested citation
Copyright
Home / Training / Manuals / Using HPV tests for cervical cancer screening and managing HPV-positive women – a practical online guide / Learning
Using HPV tests for cervical cancer screening and managing HPV-positive women – a practical online guide
Filter by language: English / Français / EspañolDifferent approaches to screening and treatment of cervical precancer | Click on the pictures to magnify and display the legends |
Cervical cancer screening aims to detect the disease in asymptomatic and apparently healthy women at a premalignant stage, when treatment of the disease is simple and can prevent progression to cancer. The paradigm of cervical cancer screening and management of precancers is evolving rapidly. Most high-income countries have achieved a significant reduction in cervical cancer incidence by screening the population with Pap smear cytology and appropriate management of screen-detected precancers. However, high-quality cytology has been difficult to implement in countries with limited resources. Given the limitations of cytology, the 2013 WHO guidelines for screening and treatment of precancerous lesions for cervical cancer prevention recommended VIA as the screening test of choice for such settings.
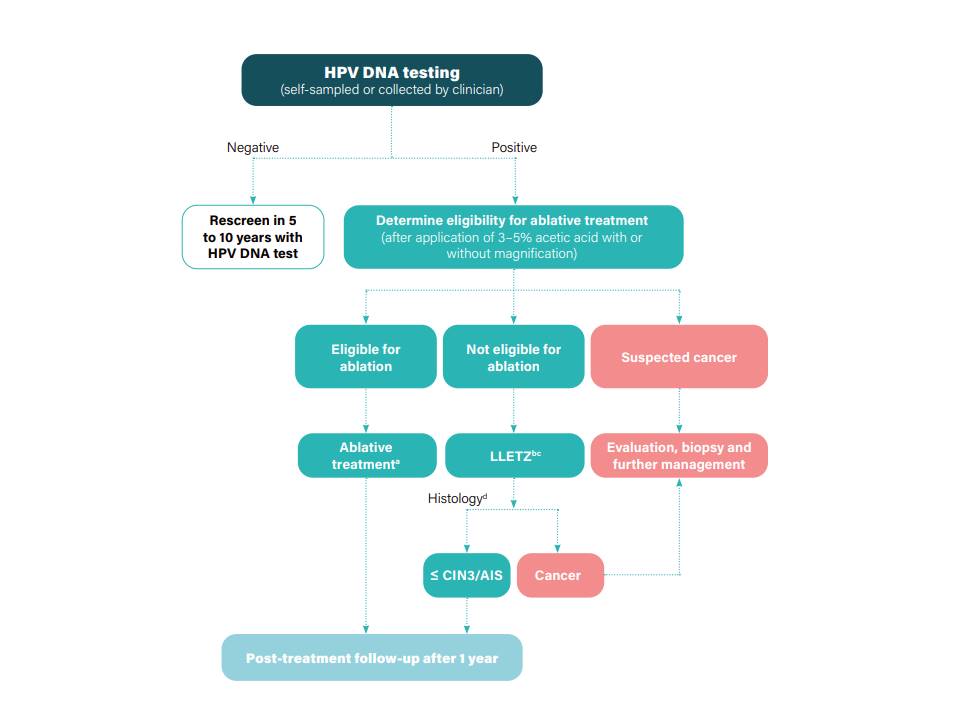
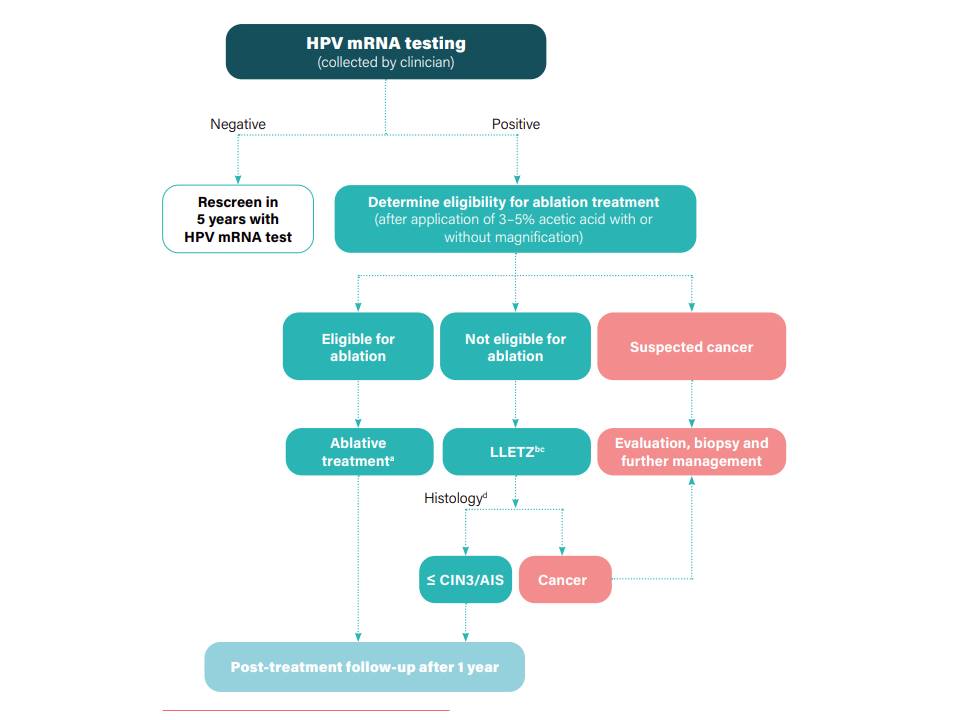
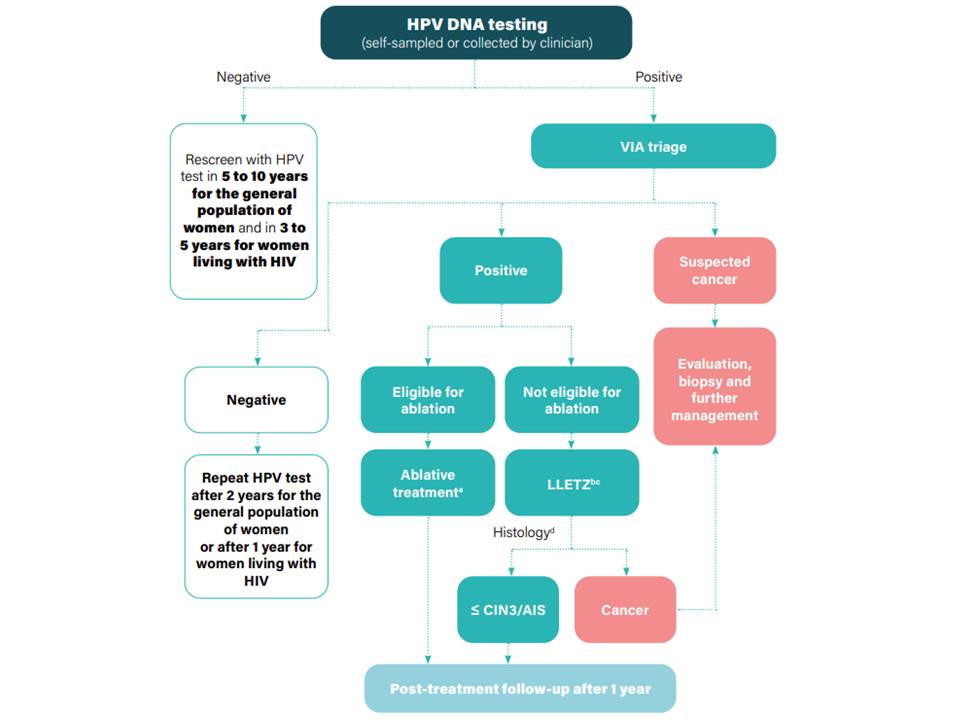
The latest WHO guideline for screening and treatment of cervical pre-cancer lesions for cervical cancer prevention, second edition (2021) strongly recommends using HPV detection as the test of choice rather than VIA or cytology; a screen-and-treat approach is recommended for HPV-positive women in the general population, and a screen, triage, and treat approach is preferred for women living with HIV. In a screen-and-treat approach, women are screened, with either an HPV test or VIA, and assessed for immediate treatment if the test result is positive. Confirmation of disease with colposcopy or histopathology is not necessary in a screen-and-treat approach, which is more suitable for low-resource settings. The greatest advantage of the screen-and-treat approach is that the women do not have to visit health facilities repeatedly, which improves their compliance with treatment. The main limitation of this approach is that a significant number of women are treated unnecessarily, because many of the HPV-positive women will not have cervical precancer (a false-positive test result). The false-positivity rate of the HPV test is particularly high in women living with HIV (WHIV). A screen-and-treat approach with an HPV test may lead to 40–50% of WHIV requiring treatment; this is not suitable for women living with HIV, and therefore WHO recommends following the screen, triage, and treat strategy (described later) for women living with HIV. When an HPV test is used for cervical cancer screening, a second test may be used to further evaluate an HPV-positive woman for the presence of cervical neoplasia. Treatment is offered only to women who have a positive result on the second test. The second test is known as the triage test, and the procedure is known as the screen, triage, and treat approach. VIA is one of the triage tests recommended by WHO after a positive HPV test result, especially for women living with HIV. Countries with adequate resources may use cytology to triage HPV-positive women, and only those HPV-positive women with abnormal cytology are referred for colposcopy for disease confirmation. Triage reduces the number of women who require treatment by reducing the number of false-positives. HPV-positive women with a negative result on the triage test require a repeat HPV test after 1 year (especially if HIV-positive) or 2 years.
In both the screen-and-treat and screen, triage, and treat approaches, most women are treated with ablative techniques (discussed later), which are simpler and have fewer complications than excisional treatment. Whatever screening approach is used, determining eligibility for ablative treatment requires assessment of the cervix after application of dilute acetic acid. A practitioner of ablative treatment needs to follow some of the basic principles and steps of VIA to determine eligibility for such treatment. Samples for HPV tests are collected by a trained provider from the cervix using a brush or a swab after exposing the cervix with a speculum. However, a woman may collect the sample for HPV testing from her upper vagina by inserting the swab herself. This procedure is called self-collection of samples, and the accuracy of this form of HPV test is almost as high as that of a test performed with a practitioner-collected sample (discussed later).
For health professionals involved in an HPV detection-based screening programme that recommends either treatment of all HPV-positive women (a screen-and-treat approach) or triage of HPV-positive women with VIA, the knowledge of principles and techniques of VIA is essential. Such health professionals are advised to also read the “Atlas of visual inspection of the cervix with acetic acid for screening, triage, and assessment for treatment”. |
IARC, 150 Cours Albert Thomas, 69372 Lyon CEDEX 08, France - Tel: +33 (0)4 72 73 84 85 - Fax: +33 (0)4 72 73 85 75
© IARC 2026 - All Rights Reserved.
© IARC 2026 - All Rights Reserved.