Introduction
Different approaches to screening and treatment of cervical precancer
Anatomical considerations
Physiological changes of the cervical epithelium
Neoplastic changes of the cervical epithelium
HPV tests – Variation between tests
Instruments, consumables, and setup required
Procedure to collect samples for HPV testing
Interpretation of HPV test results
Management of women with a positive HPV test result
Treatment of cervical intraepithelial neoplasia – principles
Steps to determine eligibility for ablative treatment
Role of Lugol’s iodine in identifying the transformation zone for treatment
Treatment by cryotherapy
Treatment by thermal ablation
Using an HPV test as the test of cure in women treated for cervical abnormalities or cervical intraepithelial neoplasia (CIN)
Infection prevention
Case studies
VIA triage outcome (applicable in screen-and-treat setting only) – negative cases
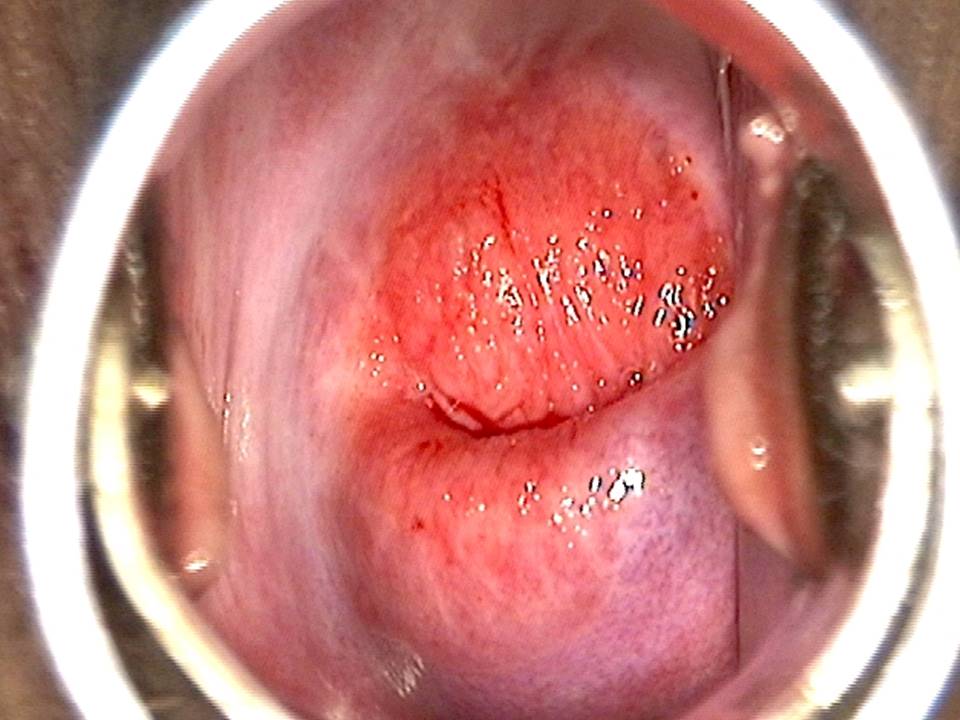
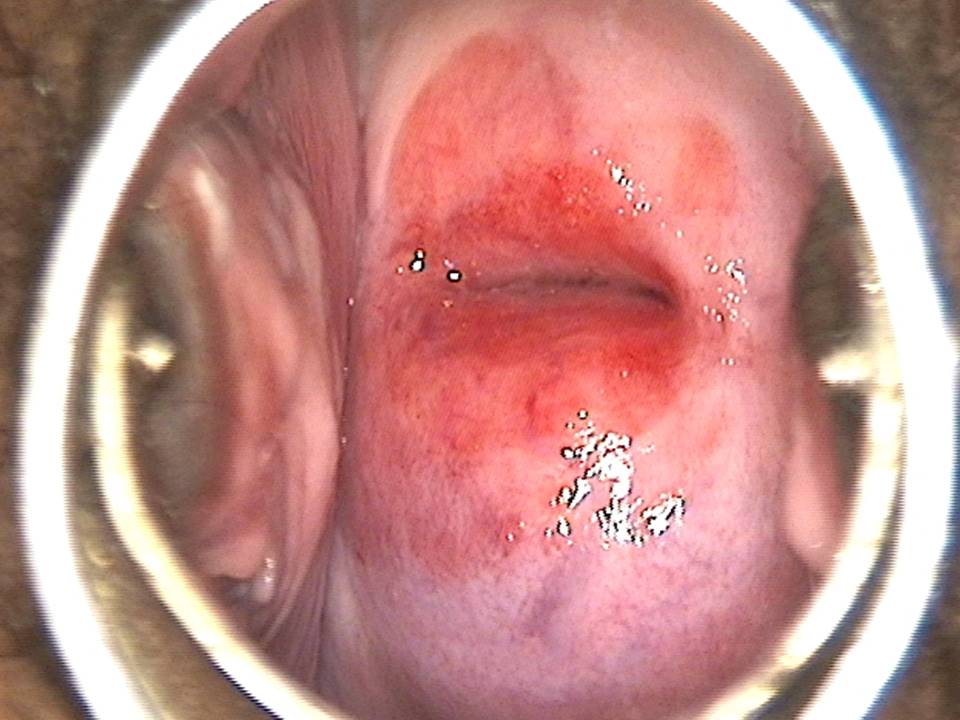
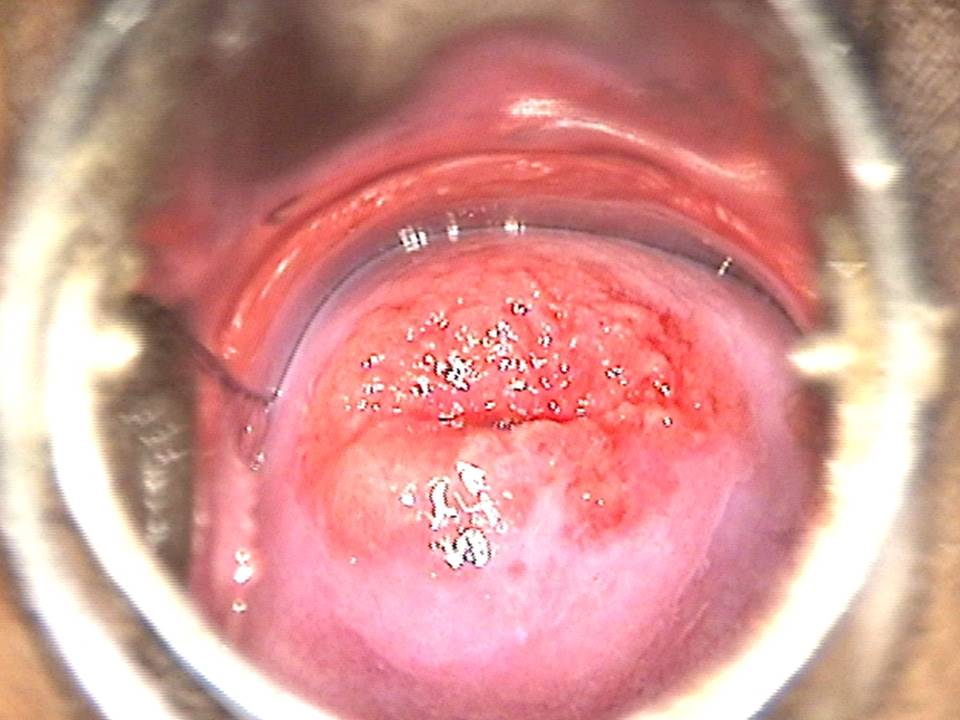
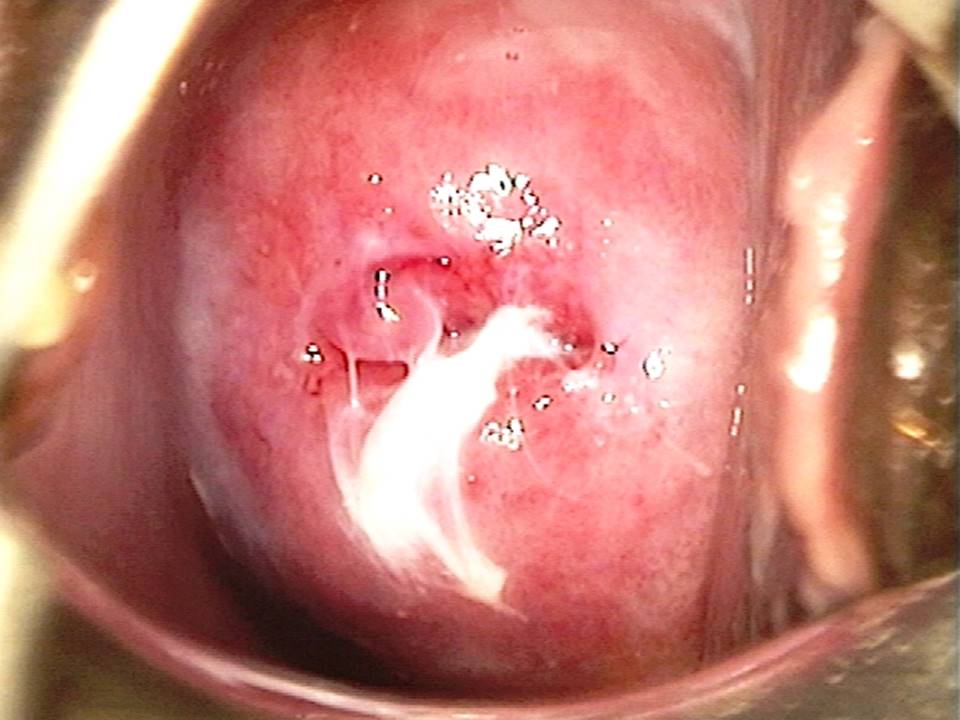
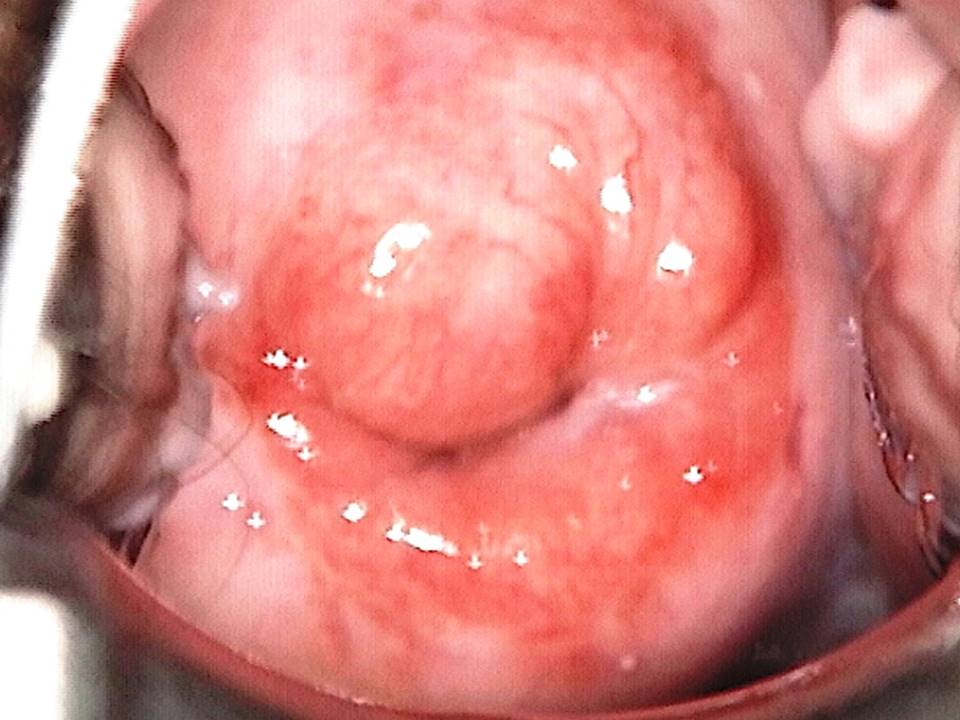
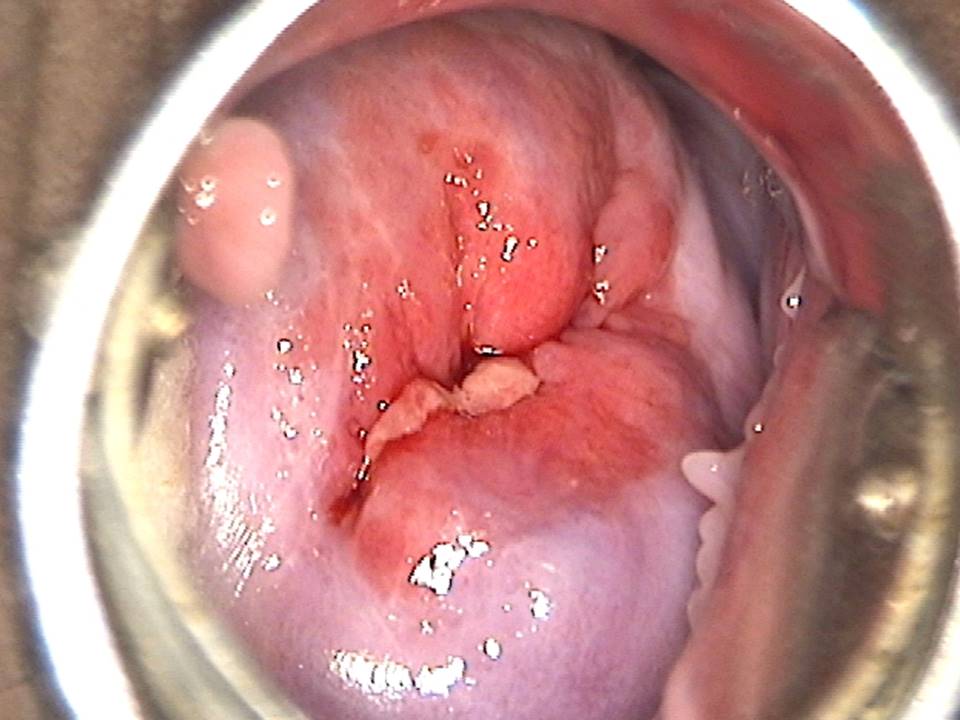
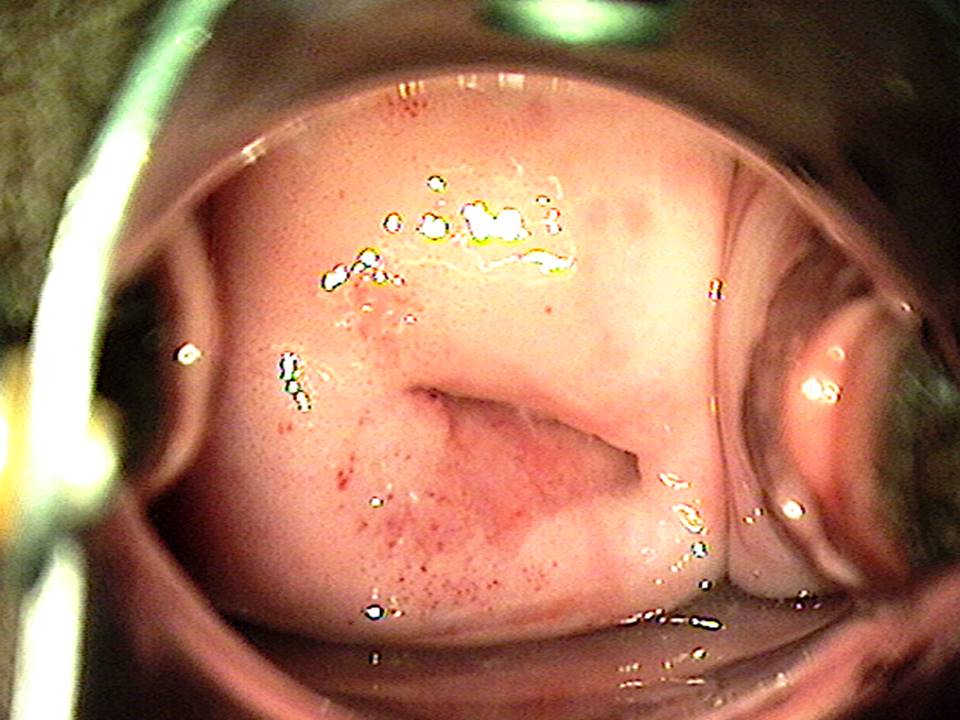
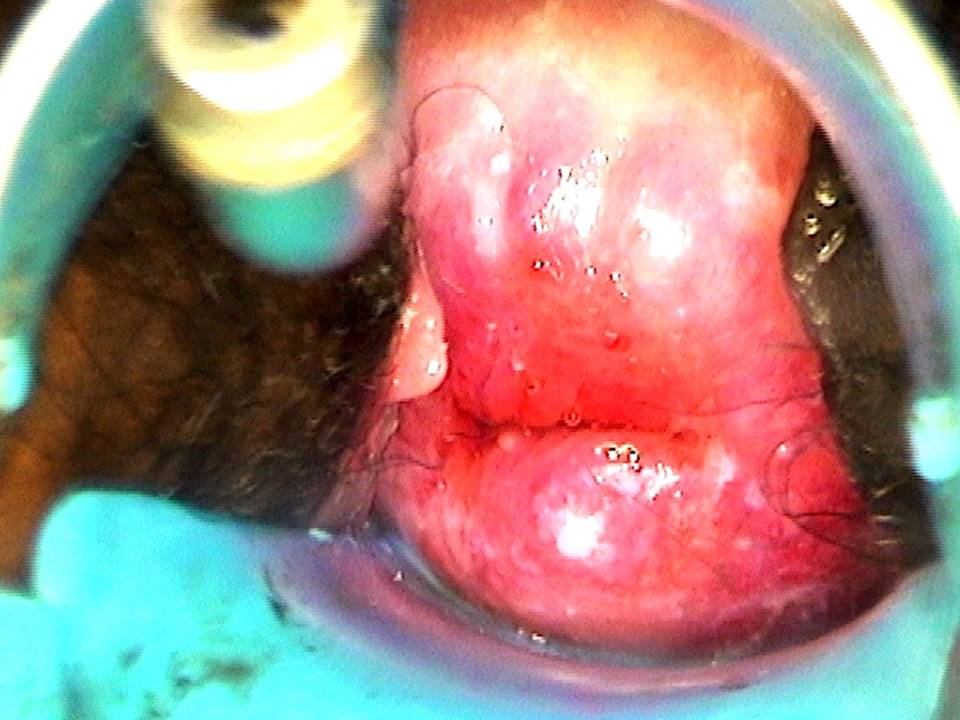
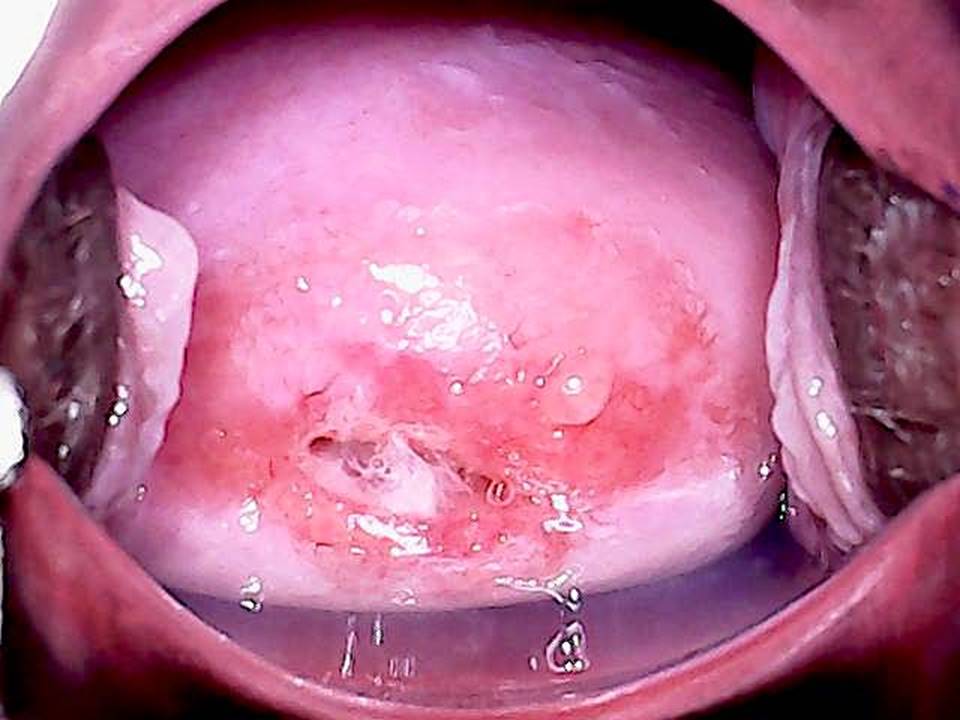
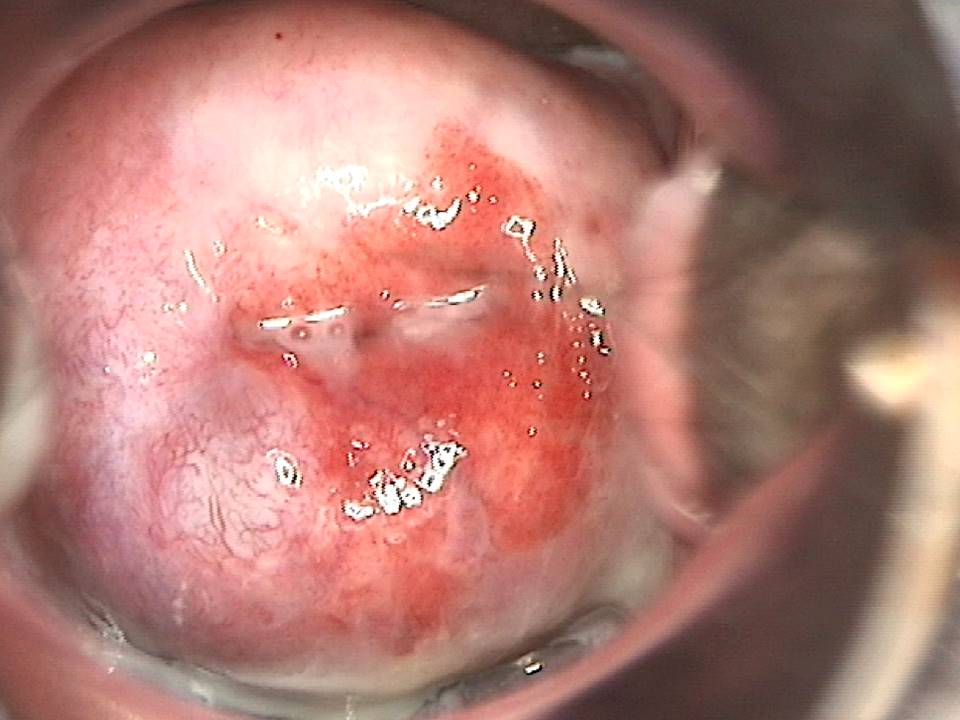
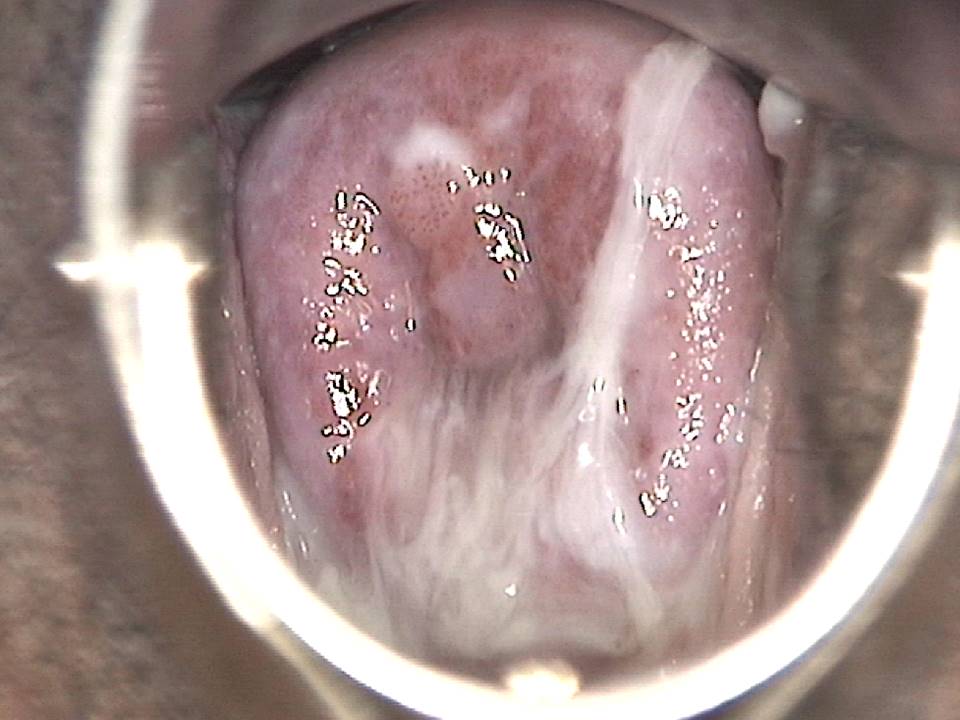
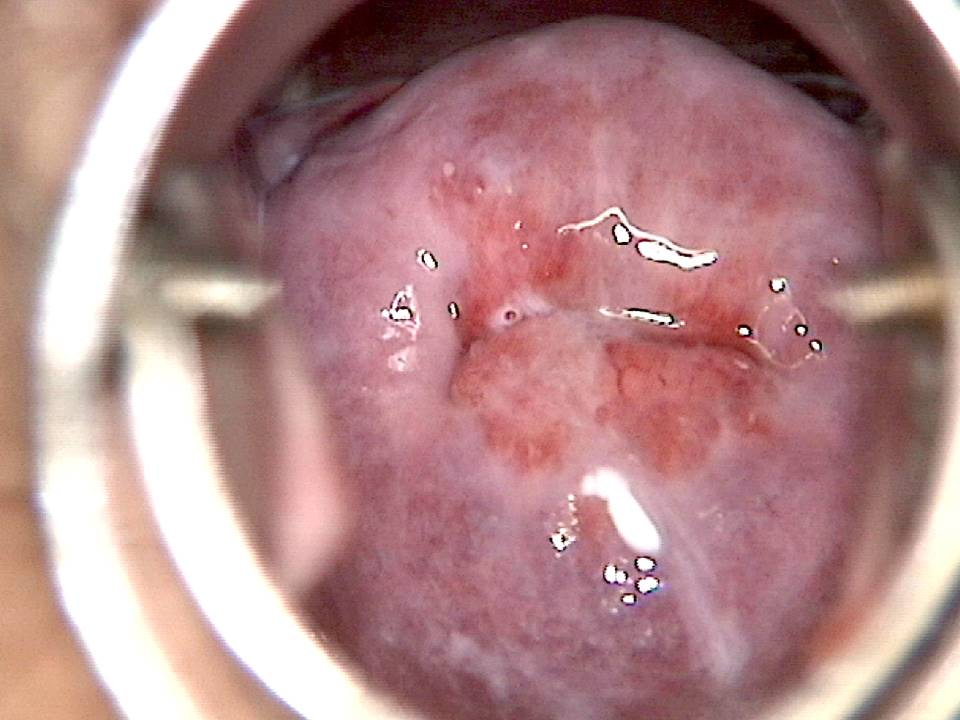
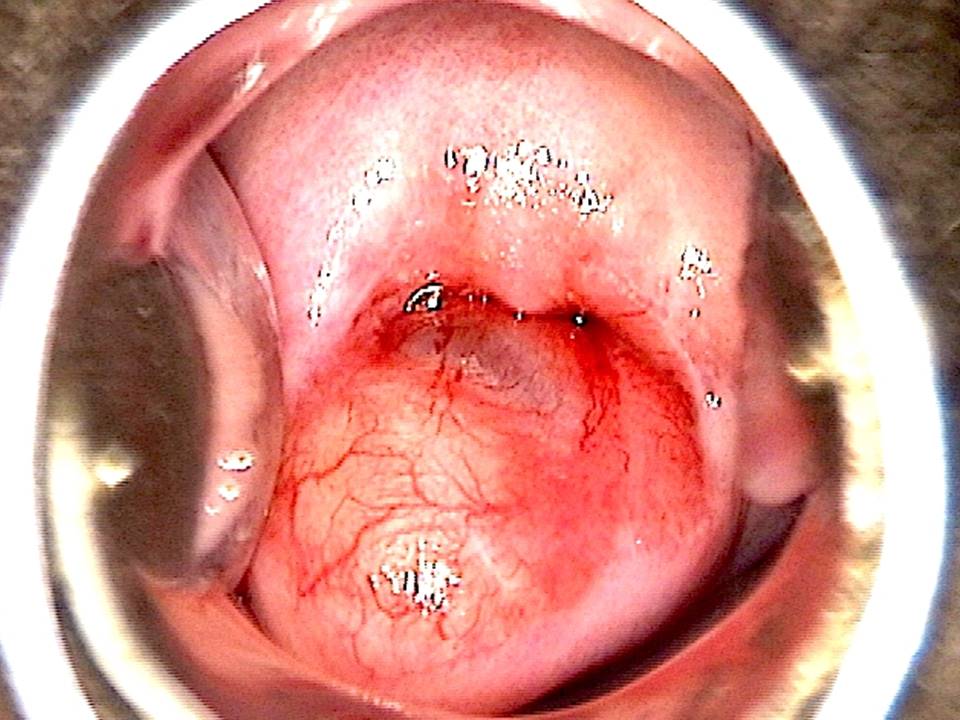
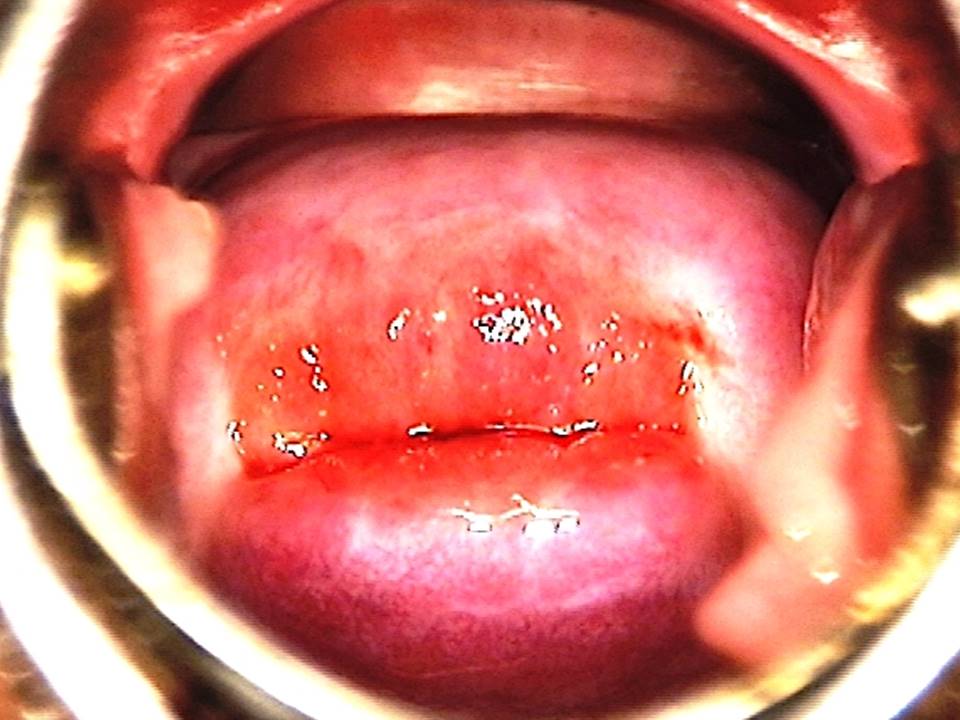
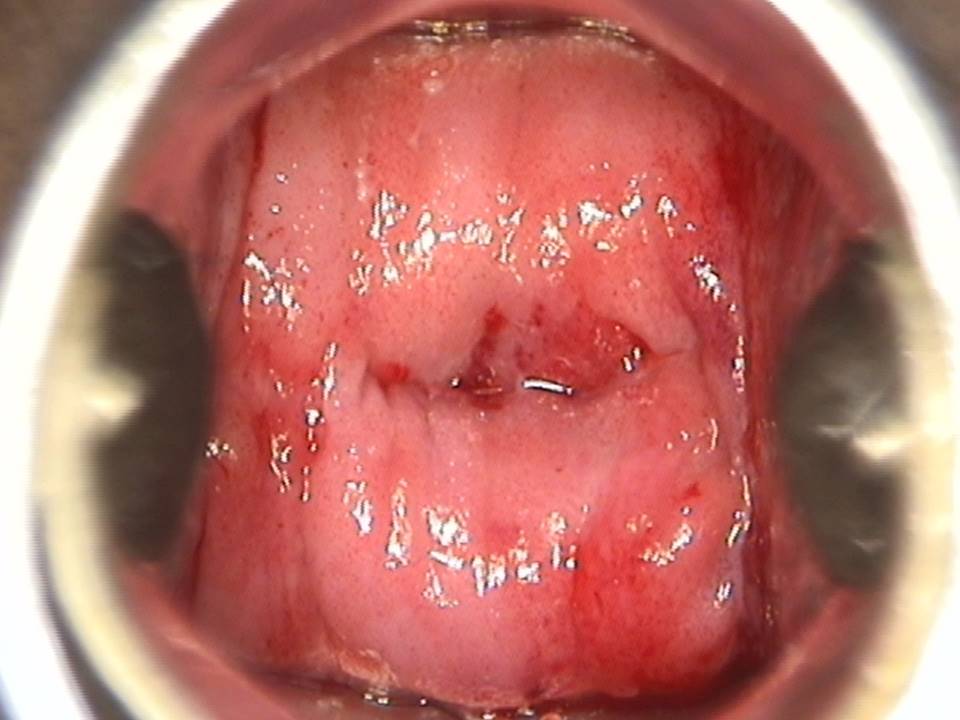
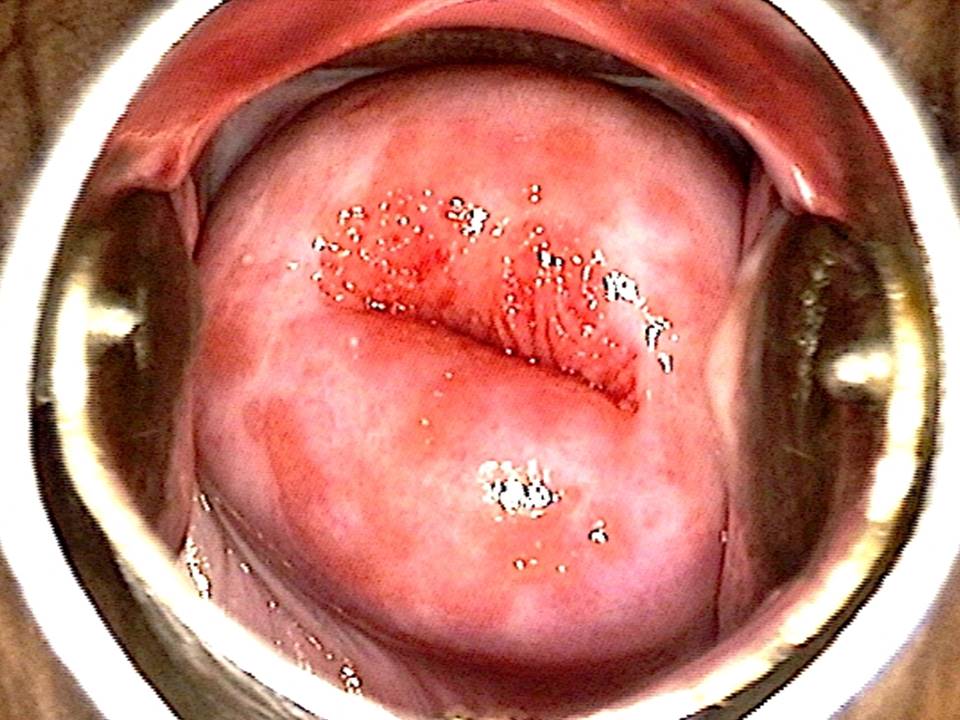
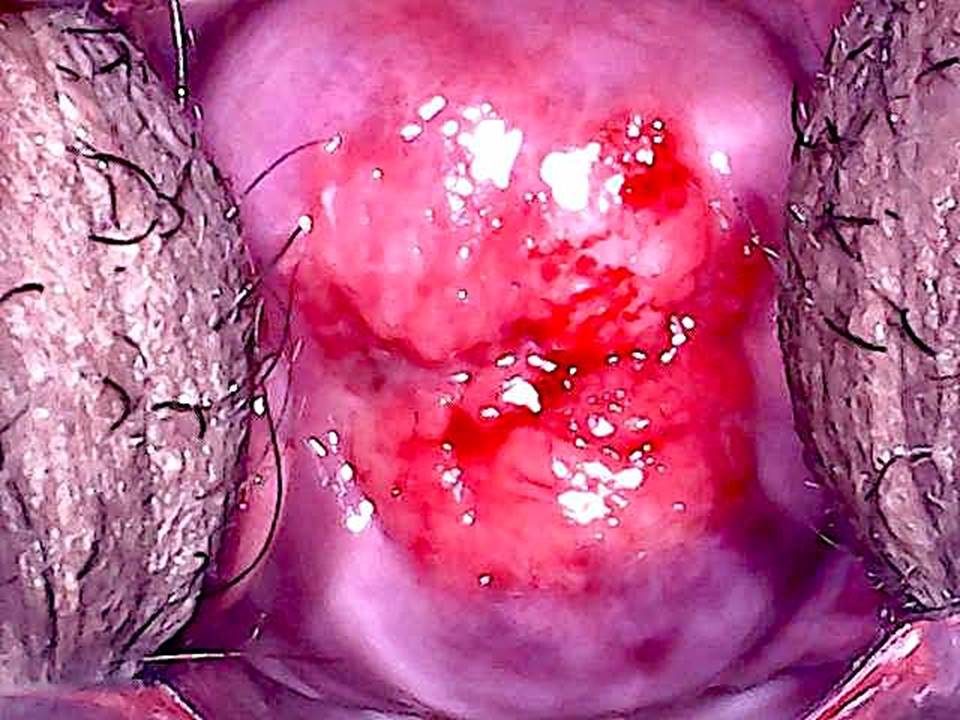
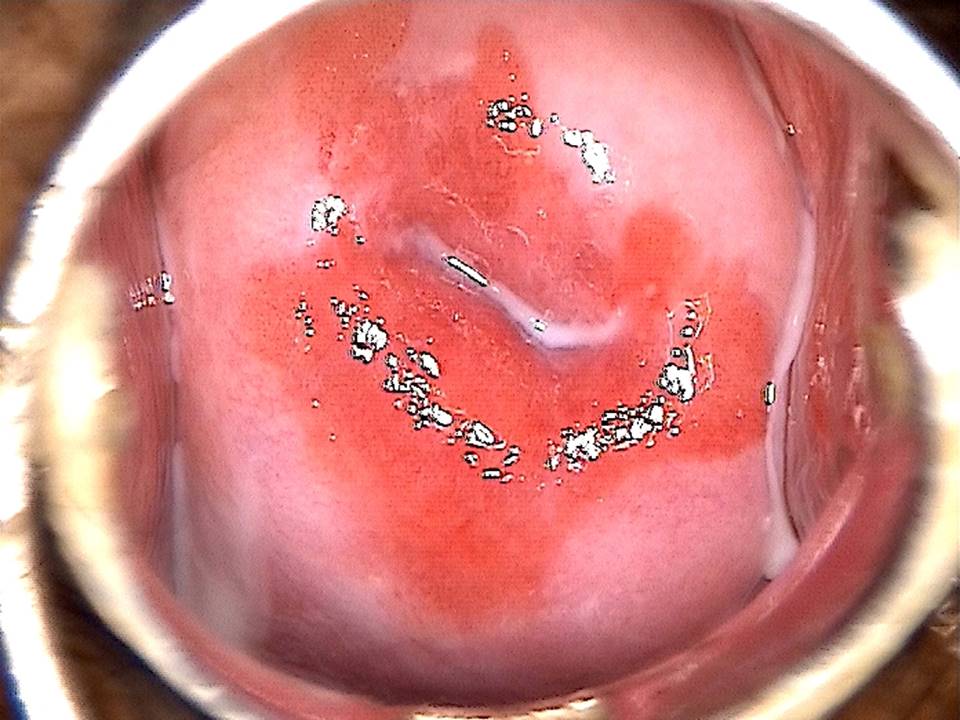
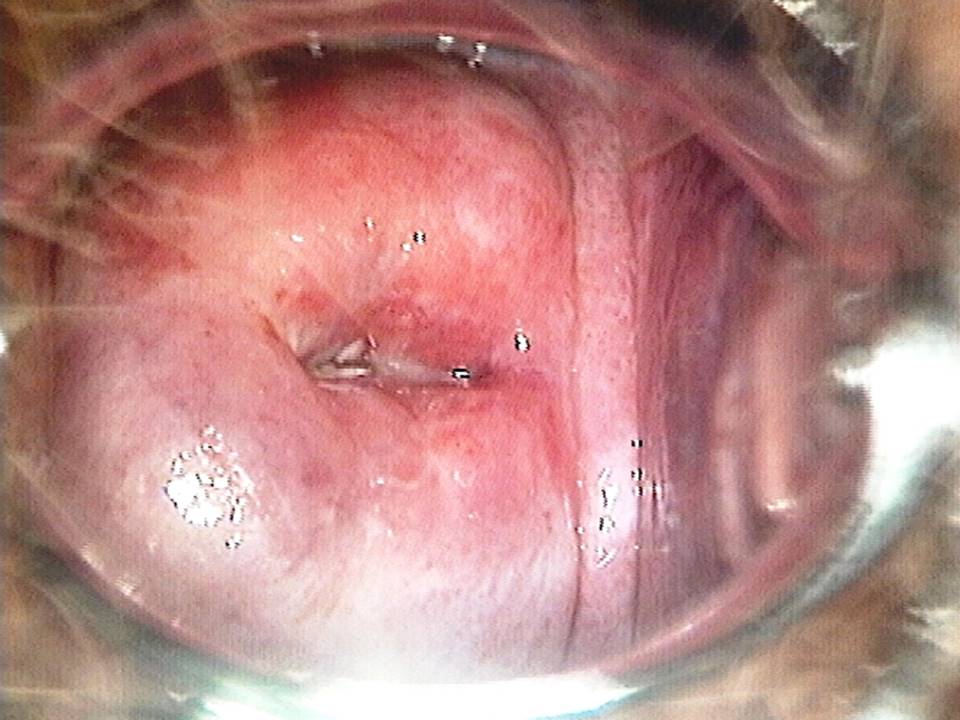
VIA triage outcome – positive cases
VIA triage outcome – suspicious of cancer cases
Foreword
Acknowledgement
Authors
Suggested citation
Copyright
Home / Training / Manuals / Using HPV tests for cervical cancer screening and managing HPV-positive women – a practical online guide / Case study
Case studies: VIA triage outcome – positive cases
Click on the following link to view examples of VIA triage outcome negative, positive or suspicious of cancer cases.
 Click to return to the atlas
Click to return to the atlas
Using HPV tests for cervical cancer screening and managing HPV-positive women – a practical online guide
Filter by language: English / Français / EspañolCase studies: VIA triage outcome – positive cases  Click to return to the atlas
Click to return to the atlas
Click on the following link to view examples of VIA triage outcome negative, positive or suspicious of cancer cases.