Introduction
Different approaches to screening and treatment of cervical precancer
Anatomical considerations
Physiological changes of the cervical epithelium
Neoplastic changes of the cervical epithelium
HPV tests – Variation between tests
Instruments, consumables, and setup required
Procedure to collect samples for HPV testing
Interpretation of HPV test results
Management of women with a positive HPV test result
Treatment of cervical intraepithelial neoplasia – principles
Steps to determine eligibility for ablative treatment
Role of Lugol’s iodine in identifying the transformation zone for treatment
Treatment by cryotherapy
Treatment by thermal ablation
Using an HPV test as the test of cure in women treated for cervical abnormalities or cervical intraepithelial neoplasia (CIN)
Infection prevention
Case studies
VIA triage outcome (applicable in screen-and-treat setting only) – negative cases
VIA triage outcome – positive cases
VIA triage outcome – suspicious of cancer cases
Foreword
Acknowledgement
Authors
Suggested citation
Copyright
Home / Training / Manuals / Using HPV tests for cervical cancer screening and managing HPV-positive women – a practical online guide / Learning
Using HPV tests for cervical cancer screening and managing HPV-positive women – a practical online guide
Filter by language: English / Français / EspañolNeoplastic changes of the cervical epithelium – Cervical intraepithelial neoplasia (CIN) | Click on the pictures to magnify and display the legends |
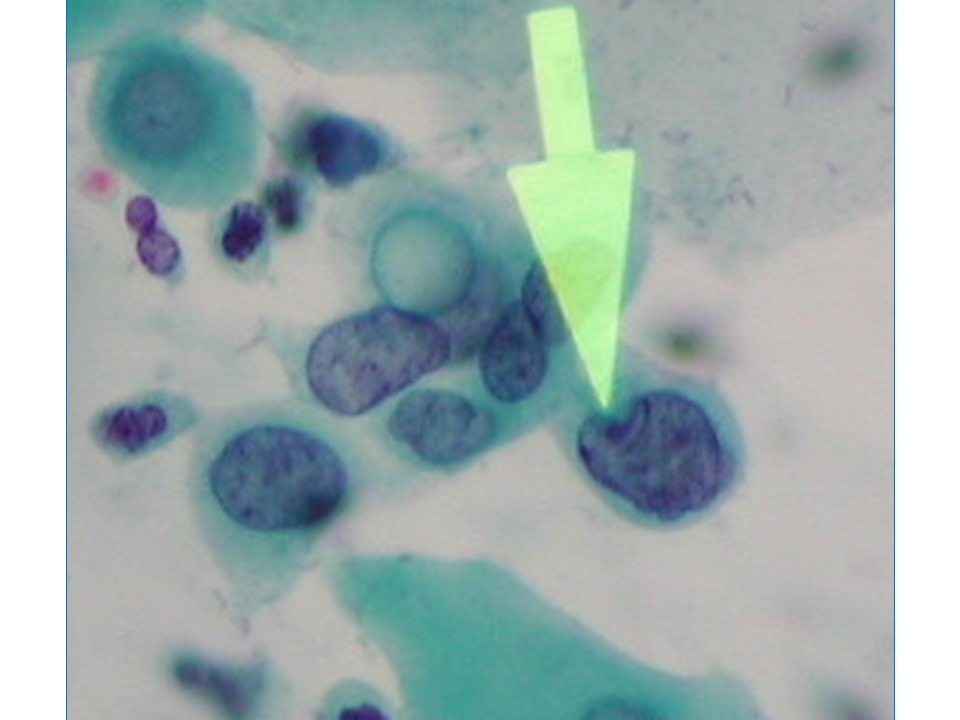
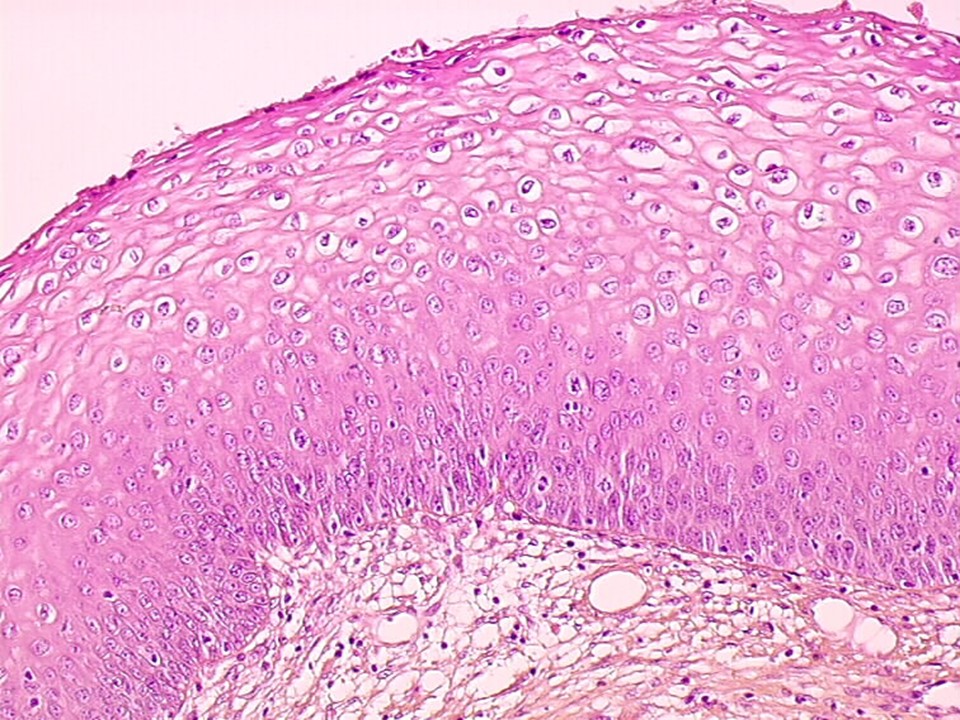
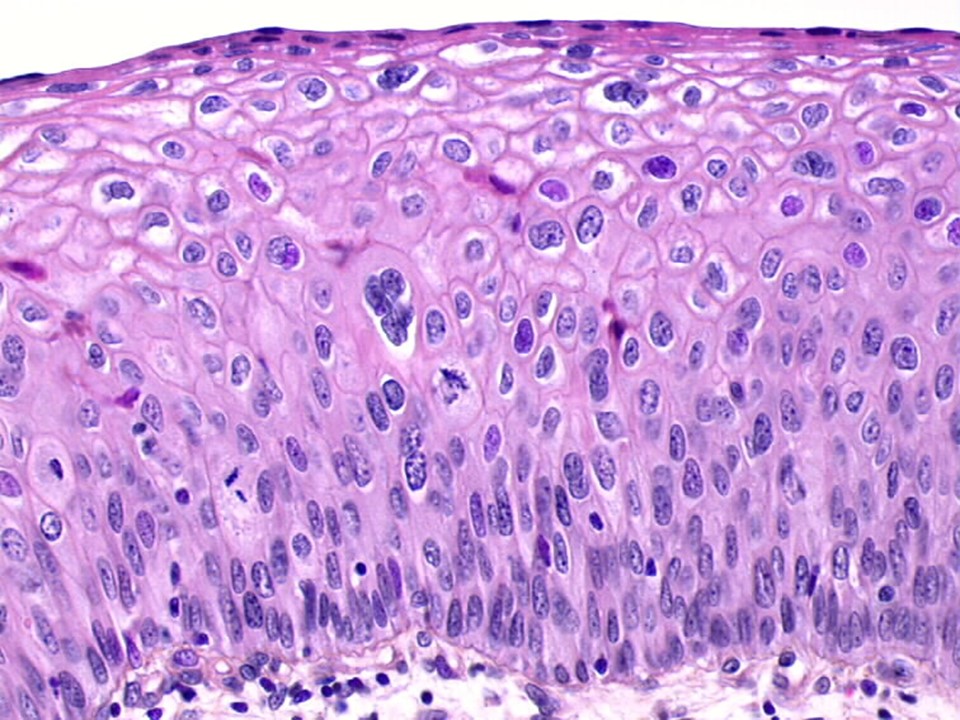
Cervical intraepithelial neoplasia (CIN) is a precancerous condition because the abnormalities are restricted to the thickness of the squamous epithelium. The neoplastic cells do not breach the basement membrane to invade deeper into the stroma or beyond. Depending on the severity of the abnormality and the extent of involvement of the thickness of the squamous epithelium, CIN lesions are graded as CIN1, CIN2, and CIN3.
The neoplastic cells present in CIN have a higher nuclear–cytoplasmic ratio compared with normal cells, an irregular nuclear membrane, dense chromatin in the nucleus, and mitotic figures. These features increase in prominence with higher grade of neoplasia. In addition, the normal systematic arrangement of the different layers of the epithelium is lost (this is called a loss of polarity) as the cells become cancerous. CIN1 is the earliest form of CIN, in which the neoplastic cells are limited to the lower third of the thickness of the cervical epithelium. Most of these lesions are caused by a transient HPV infection and disappear with the clearance of the HPV infection. The abnormal cells have the classic features of HPV infection. These cells (also known as koilocytes) have an empty and irregular zone (a halo) around the nucleus, and the nucleus is often larger in size, with irregular borders. In CIN2 and CIN3, the cervical epithelial abnormalities extend to the middle third and the upper third of the thickness of the cervical epithelium, respectively, and the cellular abnormalities become progressively more severe. The rapidly dividing abnormal cells cannot accumulate glycogen, and the cytoplasm remains intact. CIN1 lesions rarely progress to invasive cancer, but about 30–50% of CIN3 lesions will progress to invasive cancer if left untreated. The potential of CIN2 to progress further is somewhere between that of CIN1 and that of CIN3. CIN1 lesions are also known as low-grade squamous intraepithelial lesions (LSIL), because of the low potential for progression. CIN2 and CIN3 lesions are grouped together as high-grade squamous intraepithelial lesions (HSIL).
The next section provides more information about glandular precancers: adenocarcinoma in situ. |
IARC, 150 Cours Albert Thomas, 69372 Lyon CEDEX 08, France - Tel: +33 (0)4 72 73 84 85 - Fax: +33 (0)4 72 73 85 75
© IARC 2025 - All Rights Reserved.
© IARC 2025 - All Rights Reserved.