| Study sites: | India: Chennai, New Delhi, Kolkata, Thailand: Bangkok |
| Principal investigator (PI) from IARC: | P. Basu |
| PIs from collaborating institutions: |
- Dr Neerja Bhatla, All India Institute of Medical Sciences, New Delhi, India
- Dr J.S. Malliga, Cancer Institute (WIA) Chennai, Chennai, India
- Dr Ranajit Mandal, Chittaranjan National Cancer Institute (CNCI), Kolkata, India
- Dr Suleeporn Sangararang, National Cancer Institute, Bangkok, Thailand
|
| Map: | 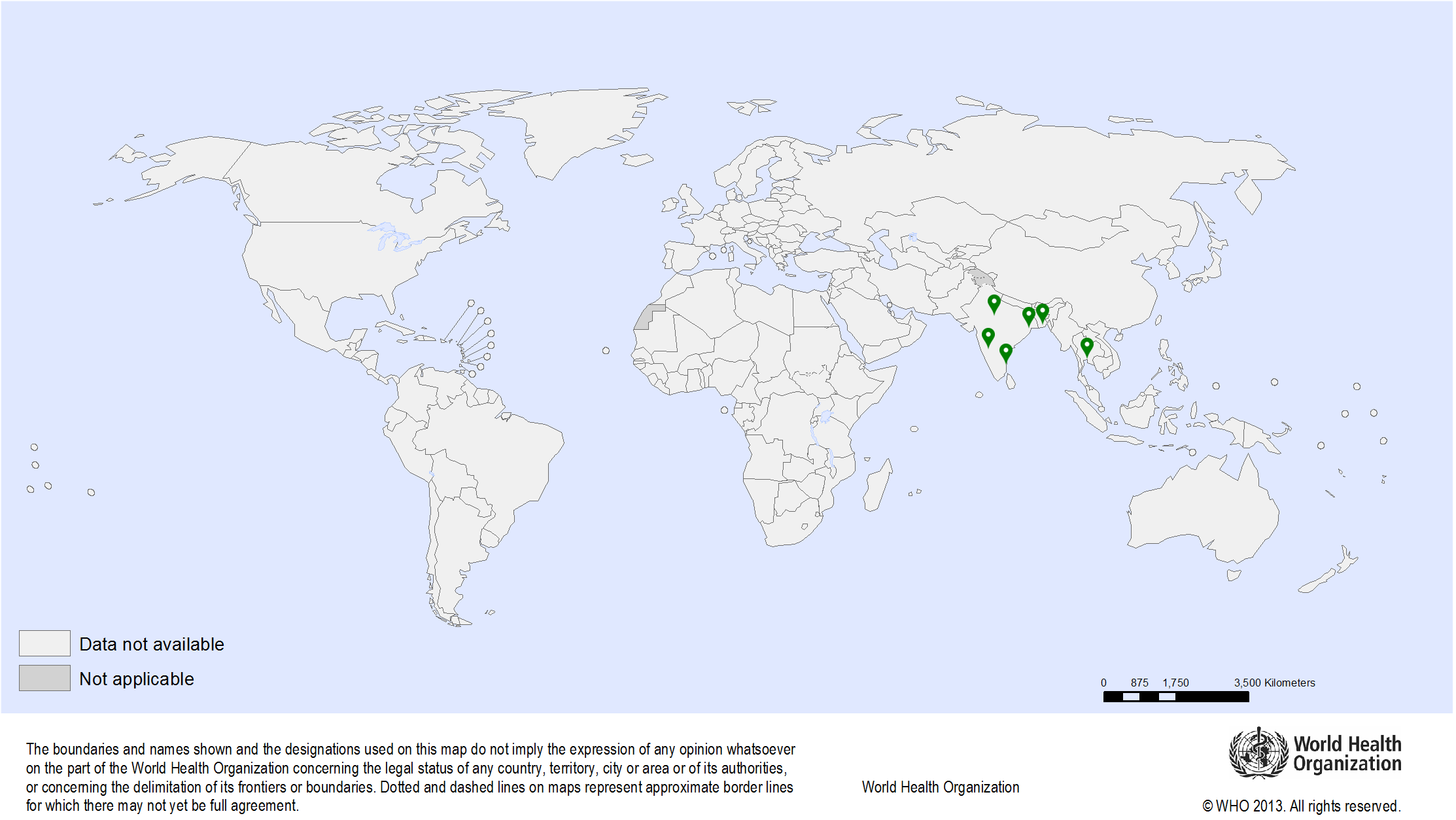
|
| Start date: | 2021 |
| Closure date: | Ongoing |
| Objectives: |
- To determine the test characteristics of Automated Visual Evaluation in a screening context:
- To estimate the sensitivity and specificity of Automated Visual Evaluation to detect cervical intraepithelial neoplasia (CIN) 2 or worse (HSIL) compared to high risk HPV testing where both are a primary screening technique.
- To determine the test characteristics of Automated Visual Evaluation in a triage context:
- To estimate and compare the sensitivity and specificity of Automated Visual Evaluation to detect CIN 2 or worse when compared to colposcopy as a triaging technique of HPV positive women.
- To compare the relative value of Automated Visual Evaluation as a diagnostic tool in screen positive women:
- To compare the efficacy of Automated Visual Evaluation with colposcopy in correctly discriminating between the CIN 2+ and normal/low-grade CIN lesions in HPV+ve women.
- To assess the efficacy of Automated Visual Evaluation in correctly defining the Transformation Zone type and thus eligibility for ablation or excision) in women requiring treatment.
|
| Methodology: |
- The Indian study sites screen 30-59-year-old women using HPV testing. In these centres screen positive women are evaluated with colposcopy prior to treatment. The present study will be integrated to these existing screening programme.
- The study will be implemented in screening settings in India and colposcopy clinics in Thailand:
- In Thailand the study will be implemented at the colposcopy clinic where women with positive HPV test and cytology test are referred for colposcopy.
Images of the cervix will be captured with the Automated Visual Evaluation device. The AI built into the device will interpret the images and decide on the location of SCJ, type of TZ, presence of abnormal lesions, the most appropriate site for biopsy and suitability for ablative treatment (based on TZ type, size and grade of lesion), but the clinician will be blinded to these outcomes. The clinician will independently document the visibility and location of the SCJ, type of TZ, Swede score, most appropriate site for taking biopsy (if any abnormalities are present) and suitability for treatment by ablation. At the end of the examination the clinician will take at least one punch biopsy from the most abnormal site determined by him/her based on Swede score (>=5). The examining clinician will be blinded to all information collected by the device until the end of the study. |
| Funding: | Intramural funds from IARC |