Home / Training / Manuals / A practical manual on visual screening for cervical neoplasia / Testing and reporting the results of visual inspection with Lugol's iodine (VILI)
Filter by language: English / Français / Español / Turkish / /
/ 
Instruments and materials required
Preparation of Lugol's iodine
Dissolve 10 g of potassium iodide in 100 ml distilled water. Add 5 g of iodine after the potassium iodide is fully dissolved. Stir well until all the iodine flakes have fully dissolved.
The solution should be stored in a sealed container to prevent evaporation of iodine and loss of staining activity.
Test provider skills
The test provider must have a good knowledge on the anatomy, physiology and pathology of the cervix in relation to its visual examination. He/she should know the clinical features of benign conditions, inflammation, precancerous lesions and invasive cancer of the cervix.
Procedure
Women coming for testing should have the screening procedure explained to them in detail. Written informed consent should be obtained before screening. An example of a written informed consent form is given in Appendix 2. Relevant obstetric and gynaecological history should be obtained and recorded with the help of a form for this purpose (Appendix 3). The woman should be reassured that the procedure is painless, and every effort should be made to ensure that she is fully relaxed and remains at ease during testing.
The woman is invited to lie down in a modified lithotomy position on a couch with leg rests or knee crutches. After proper positioning of the woman, observe if there is any vaginal discharge. Observe the external genitalia, and perineal region for any signs of excoriations, oedema, vesicles, papules, sores, ulceration and warts. Look for any swelling in the inguinal/femoral region.
Afterwards, gently introduce a sterile vaginal speculum, which has been immersed in warm water, and open the blades of the speculum to view the cervix. Adjust the light source so that there is adequate light in the vagina and on the cervix. As the speculum is gently opened and the lips are fixed, the cervix comes into view. Observe the size and shape of the cervix.
Identify the external os, columnar epithelium (red in colour), squamous epithelium (pink) and the squamocolumnar junction. Proceed to identify the transformation zone, the upper limit of which is formed by the squamocolumnar junction. Remember that cervical neoplasias occur in the transformation zone nearest to the squamocolumnar junction.
Look for ectropion, cervical polyp, nabothian cysts, healed laceration of the cervical lips, leukoplakia, condylomata and signs of cervicitis. You may note that in post menopausal women, the cervix appears pale and brittle, due to thinning and atrophy of the squamous epithelium. Assess the characteristics of discharge in terms of quantity, colour, odour and thickness. Thread-like, thin mucinous discharge from the external os indicates ovulation. Blood flow through the external os is observed in women during menstruation, and they may be subjected to VILI after 10-15 days.
In ectropion, the cervix has a large area of gross red appearance around the external os and the squamocolumnar junction is far away from the os. Nabothian cysts appear as bulging blue-white or yellow-white nodules, having a smooth delicate lining with branching blood vessels. In some women, nabothian cysts can become large and distort the shape of the cervix; however, they seldom ulcerate and become necrotic. A cervical polyp appears as a smooth mass protruding from the cervical canal beyond the external os, which may appear dark red or pink-white. Sometimes a necrotic polyp resembles a cervical cancer. Healed lacerations appear as tears on the lips of the cervix, with the external os appearing irregular. Leukoplakia appears as a smooth-surfaced, white area on the cervix that cannot be removed or scraped off. Cervical condylomata appear as raised, grey-white areas within, or outside, the transformation zone in the squamous epithelium and may be accompanied by similar lesions in the vagina and vulva.
Look for the presence of blisters with fluid or small ulcers on the cervix. Extensive erosive red areas may be present in the cervix, extending to the vagina in instances of severe cervical infection and inflammation. Observe whether there is any bleeding from the cervix, especially on touch, or ulceroproliferative growth. A very early invasive cancer may present as a rough, reddish, granular area, that may bleed on touch. More advanced invasive cancers may present as a large exophytic growth with an ulceroproliferative, bulging mass with polypoid or papillary excrescences, arising from the cervix or as a predominantly ulcerating growth replacing most of the cervix. In both of these types, bleeding on touch and necrosis are predominant clinical features. Foul-smelling discharge is also common due to superadded infection. Occasionally, invasive cancer can present as an infiltrating lesion with a grossly enlarged irregular cervix.
After carefully recording down the visual findings, liberally and gently apply Lugol's iodine with a cotton swab on the cervix. Take care not to stain either the woman's or your own clothes with iodine! After removing the swab, carefully look at the cervix for any iodine non-uptake (non-staining) areas in the form of pale or yellowish-white areas, particularly in the transformation zone, close to the squamocolumnar junction. Once the examination is completed, the excess iodine in the vaginal fornices should be mopped up with dry cotton.
Conclusion of the examination
Contaminated swabs, gauze and other waste material should be disposed of in the plastic bag in a plastic bucket.
Withdraw the speculum gently, and inspect the vaginal walls for condyloma and iodo-negative lesions. Before removing the soiled gloves, immerse the hands briefly in a container filled with 0.5% chlorine solution. Decontaminate the used gloves by soaking in the 0.5% chlorine in a plastic bucket for 10 minutes. Preparation of 0.5% chlorine solution is described in Appendix 4.
The speculum and other instruments used during VILI should be immersed in 0.5% chlorine solution for 10 minutes' decontamination, before cleaning with water. The cleaned instruments may be reused after high-level disinfection by immersing them in boiling water for 20 minutes or by sterilizing the instruments using an autoclave.
Documentation of findings and advising the woman
Carefully document the outcome of testing in the reporting form (Appendix 3). Explain the outcome of the test to the woman, as well as any further course of follow-up actions. If the test is negative, the woman is reassured and she may be advised to repeat testing after five years. If the test is positive, she should be referred for further investigations such as colposcopy and biopsy as well as treatment for any confirmed lesions. If invasive cancer is suspected, she should be referred to a cancer diagnosis and treatment facility.
Reporting the outcome of VILI
The patterns associated with the outcomes after VILI are shown in Figures 3.1-3.21.
VILI negative (-)
VILI screening is reported as negative in the case of any of the following observations after iodine application:

fig 3.2: VILI negative: The squamous epithelium is black and the columnar epithelium does not change colour after the application of iodine.
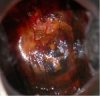
fig 3.3: VILI negative: There are patchy, ill-defined, scattered non-iodine uptake areas in the cervix; these are not restricted to the transformation zone. This appearance is due to inflammation of the cervix.
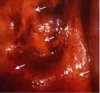
fig 3.4: VILI negative: There are patchy, ill-defined areas of iodine non-uptake (narrow arrows) and partial iodine uptake (dense arrows).
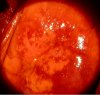
fig 3.5: VILI negative: Squamous epithelium remains brown. There are patchy areas of no or partial uptake of iodine in the transformation zone corresponding to areas of immature squamous metaplasia and inflammation.

fig 3.6: VILI negative: There are patchy, ill-defined areas of iodine non-uptake (narrow arrow) and partial iodine uptake (dense arrows).
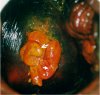
fig 3.7: VILI negative: There are areas of iodine non-uptake (narrow arrow) and partial uptake (dense arrow) in the polyp. Squamous epithelium is black.

fig 3.8: VILI negative: There are patchy areas of iodine non-uptake, scattered all over the cervix, not restricted to the transformation zone. This is characteristic of chronic cervicitis.

fig 3.9: VILI negative: There are pepper-like areas of iodine non-uptake in the squamous epithelium, due to cervical ulceration following inflammation.
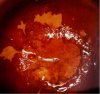
fig 3.10: VILI negative: Iodine-negative, irregular yellow areas are detached from the squamocolumnar junction and constitute ‘satellite’ lesions.
VILI positive (+)
The outcome is scored as positive if dense, thick, bright, mustard-yellow or saffron-yellow iodine non-uptake areas are seen in the transformation zone, close to or abutting the squamocolumnar junction or close to the os if the squamocolumnar junction is not seen (Figures 3.11-3.15) or when the entire cervix turns densely yellow (Figure 3.16).

fig 3.11: VILI positive: There is a saffron-yellow area of iodine non-uptake in the anterior lip abutting the squamocolumnar junction.

fig 3.12: VILI positive: There is a mustard yellow lesion with no iodine uptake in the anterior lip touching the squamocolumnar junction.
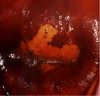
fig 3.13: VILI positive: There is a mustard-yellow area of iodine non-uptake in the anterior lip abutting the squamocolumnar junction.
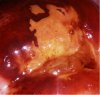
fig 3.14: VILI positive: There is a dense, mustard-yellow area of iodine non-uptake abutting the squamocolumnar junction in the anterior lip of the cervix with irregular, angular margins.

fig 3.15: VILI positive: There are large, thick, mustard yellow areas of iodine non-uptake in the upper and lower lip of cervix extending into the cervical canal.

fig 3.16: VILI positive: There is a large, dense, saffron- yellow area of iodine non-uptake with irregular surface, involving all the four quadrants and extending into the cervical canal.
VILI positive, invasive cancer
Invasive cancer is reported when a frank, nodular, irregular, ulceroproliferative growth is visible on the cervix which turns densely yellow on application of iodine (Figures 3.17-3.19).

fig 3.17: VILI positive, invasive cancer: There is a dense, thick, extensive, mustard-yellow area, with irregular and nodular surface, involving all the quadrants of the cervix. The external os is obliterated.

fig 3.18: VILI positive, invasive cancer: There is a large, thick irregular, nodular mustard-yellow lesion suggestive of invasive cancer.

fig 3.19: VILI positive, invasive cancer. There is a large, thick mustard-yellow area in the cervix with irregular, nodular surface contour.
Self-evaluation of the test providers
The test providers are encouraged to correlate the results of their VILI testing with histological findings (if done). A sufficiently skilled examiner will categorize 10-15% of women as VILI +, and 20-30% of those women will be found to harbour CIN of any grade.
A practical manual on visual screening for cervical neoplasia
Chapter 3 / Testing and reporting the results of visual inspection with Lugol's iodine (VILI)
Filter by language: English / Français / Español / Turkish /
 /
/ 
- Examination table with knee crutches or leg rests or stirrups;
- Good light source (preferably a bright halogen lamp that can be easily directed at the cervix);
- Sterile speculum: Cusco's, Grave's or Collin's;
- Pair of gloves;
- Cotton swabs; cotton-tipped buds, gauze;
- Ring forceps, pickup forceps;
- 5% Lugol's iodine solution;
- An aluminium, steel or plastic container with 0.5% chlorine solution in which to immerse the gloves;
- Plastic bucket or container with 0.5% chlorine solution for decontamination of instruments;
- A plastic bucket with a plastic bag to dispose of contaminated swabs and other waste items.
The solution should be stored in a sealed container to prevent evaporation of iodine and loss of staining activity.
The woman is invited to lie down in a modified lithotomy position on a couch with leg rests or knee crutches. After proper positioning of the woman, observe if there is any vaginal discharge. Observe the external genitalia, and perineal region for any signs of excoriations, oedema, vesicles, papules, sores, ulceration and warts. Look for any swelling in the inguinal/femoral region.
Afterwards, gently introduce a sterile vaginal speculum, which has been immersed in warm water, and open the blades of the speculum to view the cervix. Adjust the light source so that there is adequate light in the vagina and on the cervix. As the speculum is gently opened and the lips are fixed, the cervix comes into view. Observe the size and shape of the cervix.
Identify the external os, columnar epithelium (red in colour), squamous epithelium (pink) and the squamocolumnar junction. Proceed to identify the transformation zone, the upper limit of which is formed by the squamocolumnar junction. Remember that cervical neoplasias occur in the transformation zone nearest to the squamocolumnar junction.
Look for ectropion, cervical polyp, nabothian cysts, healed laceration of the cervical lips, leukoplakia, condylomata and signs of cervicitis. You may note that in post menopausal women, the cervix appears pale and brittle, due to thinning and atrophy of the squamous epithelium. Assess the characteristics of discharge in terms of quantity, colour, odour and thickness. Thread-like, thin mucinous discharge from the external os indicates ovulation. Blood flow through the external os is observed in women during menstruation, and they may be subjected to VILI after 10-15 days.
In ectropion, the cervix has a large area of gross red appearance around the external os and the squamocolumnar junction is far away from the os. Nabothian cysts appear as bulging blue-white or yellow-white nodules, having a smooth delicate lining with branching blood vessels. In some women, nabothian cysts can become large and distort the shape of the cervix; however, they seldom ulcerate and become necrotic. A cervical polyp appears as a smooth mass protruding from the cervical canal beyond the external os, which may appear dark red or pink-white. Sometimes a necrotic polyp resembles a cervical cancer. Healed lacerations appear as tears on the lips of the cervix, with the external os appearing irregular. Leukoplakia appears as a smooth-surfaced, white area on the cervix that cannot be removed or scraped off. Cervical condylomata appear as raised, grey-white areas within, or outside, the transformation zone in the squamous epithelium and may be accompanied by similar lesions in the vagina and vulva.
Look for the presence of blisters with fluid or small ulcers on the cervix. Extensive erosive red areas may be present in the cervix, extending to the vagina in instances of severe cervical infection and inflammation. Observe whether there is any bleeding from the cervix, especially on touch, or ulceroproliferative growth. A very early invasive cancer may present as a rough, reddish, granular area, that may bleed on touch. More advanced invasive cancers may present as a large exophytic growth with an ulceroproliferative, bulging mass with polypoid or papillary excrescences, arising from the cervix or as a predominantly ulcerating growth replacing most of the cervix. In both of these types, bleeding on touch and necrosis are predominant clinical features. Foul-smelling discharge is also common due to superadded infection. Occasionally, invasive cancer can present as an infiltrating lesion with a grossly enlarged irregular cervix.
After carefully recording down the visual findings, liberally and gently apply Lugol's iodine with a cotton swab on the cervix. Take care not to stain either the woman's or your own clothes with iodine! After removing the swab, carefully look at the cervix for any iodine non-uptake (non-staining) areas in the form of pale or yellowish-white areas, particularly in the transformation zone, close to the squamocolumnar junction. Once the examination is completed, the excess iodine in the vaginal fornices should be mopped up with dry cotton.
Withdraw the speculum gently, and inspect the vaginal walls for condyloma and iodo-negative lesions. Before removing the soiled gloves, immerse the hands briefly in a container filled with 0.5% chlorine solution. Decontaminate the used gloves by soaking in the 0.5% chlorine in a plastic bucket for 10 minutes. Preparation of 0.5% chlorine solution is described in Appendix 4.
The speculum and other instruments used during VILI should be immersed in 0.5% chlorine solution for 10 minutes' decontamination, before cleaning with water. The cleaned instruments may be reused after high-level disinfection by immersing them in boiling water for 20 minutes or by sterilizing the instruments using an autoclave.
The patterns associated with the outcomes after VILI are shown in Figures 3.1-3.21.
- A normal cervix; the squamous epithelium turns mahogany brown or black and the columnar epithelium does not change colour (figure 3.2).
- Patchy, indistinct, ill-defined, colourless or partially brown areas are seen (Figures 3.3-3.6).
- Pale areas of no or partial iodine uptake are present on polyps (Figure 3.7).
- A leopard-skin appearance (Figure 3.8) is associated with T. vaginalis infection.
- Pepper-like non-iodine uptake areas are seen in the squamous epithelium, far away from the squamocolumnar junction (Figures 3.9)
- Satellite, thin, yellow, non-iodine uptake areas with angular, or digitating margins, resembling geographical areas, are seen far away from the squamocolumnar junction (Figure 3.10).

fig 3.2: VILI negative: The squamous epithelium is black and the columnar epithelium does not change colour after the application of iodine.
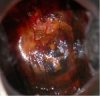
fig 3.3: VILI negative: There are patchy, ill-defined, scattered non-iodine uptake areas in the cervix; these are not restricted to the transformation zone. This appearance is due to inflammation of the cervix.
fig 3.4: VILI negative: There are patchy, ill-defined areas of iodine non-uptake (narrow arrows) and partial iodine uptake (dense arrows).
fig 3.5: VILI negative: Squamous epithelium remains brown. There are patchy areas of no or partial uptake of iodine in the transformation zone corresponding to areas of immature squamous metaplasia and inflammation.

fig 3.6: VILI negative: There are patchy, ill-defined areas of iodine non-uptake (narrow arrow) and partial iodine uptake (dense arrows).
fig 3.7: VILI negative: There are areas of iodine non-uptake (narrow arrow) and partial uptake (dense arrow) in the polyp. Squamous epithelium is black.

fig 3.8: VILI negative: There are patchy areas of iodine non-uptake, scattered all over the cervix, not restricted to the transformation zone. This is characteristic of chronic cervicitis.

fig 3.9: VILI negative: There are pepper-like areas of iodine non-uptake in the squamous epithelium, due to cervical ulceration following inflammation.
fig 3.10: VILI negative: Iodine-negative, irregular yellow areas are detached from the squamocolumnar junction and constitute ‘satellite’ lesions.

fig 3.11: VILI positive: There is a saffron-yellow area of iodine non-uptake in the anterior lip abutting the squamocolumnar junction.

fig 3.12: VILI positive: There is a mustard yellow lesion with no iodine uptake in the anterior lip touching the squamocolumnar junction.
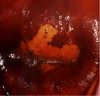
fig 3.13: VILI positive: There is a mustard-yellow area of iodine non-uptake in the anterior lip abutting the squamocolumnar junction.
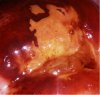
fig 3.14: VILI positive: There is a dense, mustard-yellow area of iodine non-uptake abutting the squamocolumnar junction in the anterior lip of the cervix with irregular, angular margins.

fig 3.15: VILI positive: There are large, thick, mustard yellow areas of iodine non-uptake in the upper and lower lip of cervix extending into the cervical canal.

fig 3.16: VILI positive: There is a large, dense, saffron- yellow area of iodine non-uptake with irregular surface, involving all the four quadrants and extending into the cervical canal.

fig 3.17: VILI positive, invasive cancer: There is a dense, thick, extensive, mustard-yellow area, with irregular and nodular surface, involving all the quadrants of the cervix. The external os is obliterated.

fig 3.18: VILI positive, invasive cancer: There is a large, thick irregular, nodular mustard-yellow lesion suggestive of invasive cancer.

fig 3.19: VILI positive, invasive cancer. There is a large, thick mustard-yellow area in the cervix with irregular, nodular surface contour.




