Using Human Papillomavirus (HPV) detection tests for cervical cancer screening and managing HPV-positive women – a practical guide / Activity 3
Neoplastic changes of the cervical epithelium – Genesis of precancerous lesions and cervical cancer | Click on the pictures to magnify and display the legends |
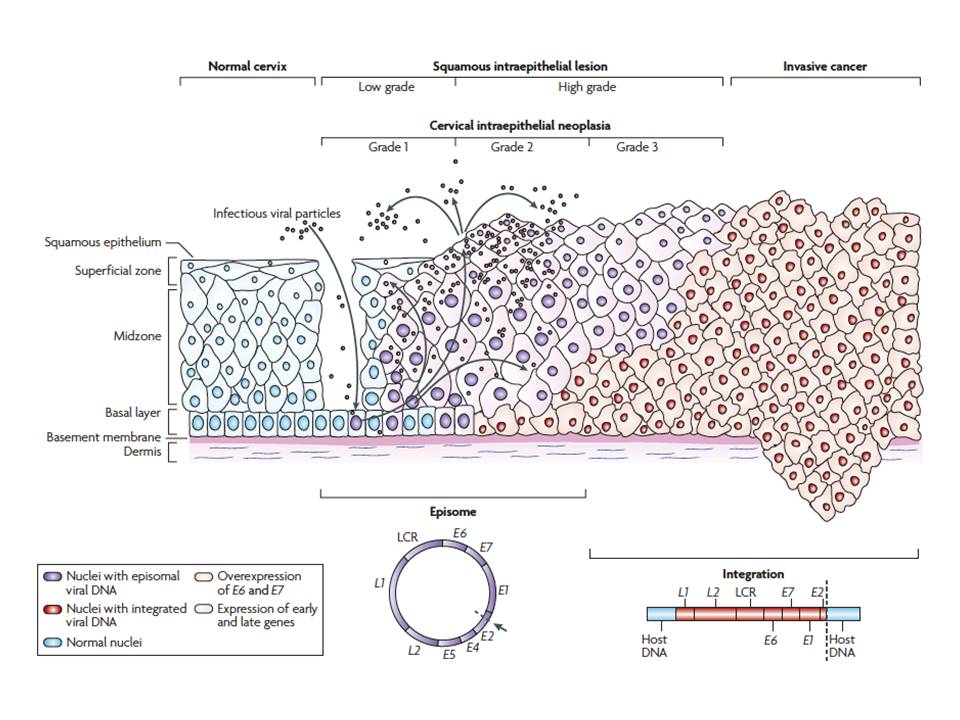
HPV enters the basal layer of cells of the squamous epithelium through micro-abrasions on the epithelium. The virus proliferates in the cytoplasm of the dividing cells and is finally shed into the vagina as the mature cervical cells exfoliate from the surface of the cervix. The shed virus can be transmitted to a sexual partner. The replicating virus in the cell cytoplasm is known as the episomal form of the virus.
Persistence of the viral infection leads to integration of viral DNA with the host-cell DNA, leading to the production of viral proteins by the host cells. Of these proteins, two types (E6 and E7) are responsible for neoplastic transformation. E6 and E7 proteins degrade the p53 and retinoblastoma (pRB) tumour suppressor genes, respectively. These tumour suppressor genes maintain normal cell division and programmed cell death (apoptosis) and thus have a protective effect against unregulated cell proliferation. Their degradation by E6/E7 proteins (also known as oncoproteins) leads to unregulated cell proliferation in the cervix, thus initiating neoplastic transformation. The persistence of high-risk HPV infection leads to the development of a premalignant condition of the squamous epithelium, known as cervical intraepithelial neoplasia (CIN). CIN is also known as squamous intraepithelial lesion (SIL). A similar premalignant lesion that develops less frequently over the columnar epithelium is known as adenocarcinoma in situ (AIS). If it remains undetected and is left untreated, CIN or AIS may lead to invasive cervical cancer after 5–10 years.
Depending on the severity and the potential for progression to invasive cancers, CIN lesions are graded as CIN1, CIN2, and CIN3. Whereas CIN1 is the earliest form of precancer, with a very low potential for progression to cancer, CIN2 and especially CIN3 have a much higher risk of progression. AIS is always considered to be a high-grade lesion, because of its high potential for progression to adenocarcinoma. Cervical cancer that develops from a CIN lesion is known as squamous cell cancer because it arises from the squamous epithelium. Squamous cell cancers comprise 80–90% of all cervical cancers. A cancer that arises due to progression of AIS in the columnar epithelium is known as adenocarcinoma. CIN and AIS may coexist and lead to the development of adenosquamous carcinoma. To learn more about CIN, please click here.
|