Using Human Papillomavirus (HPV) detection tests for cervical cancer screening and managing HPV-positive women – a practical guide / Activity 3
Neoplastic changes of the cervical epithelium – HPV structure and types | Click on the pictures to magnify and display the legends |
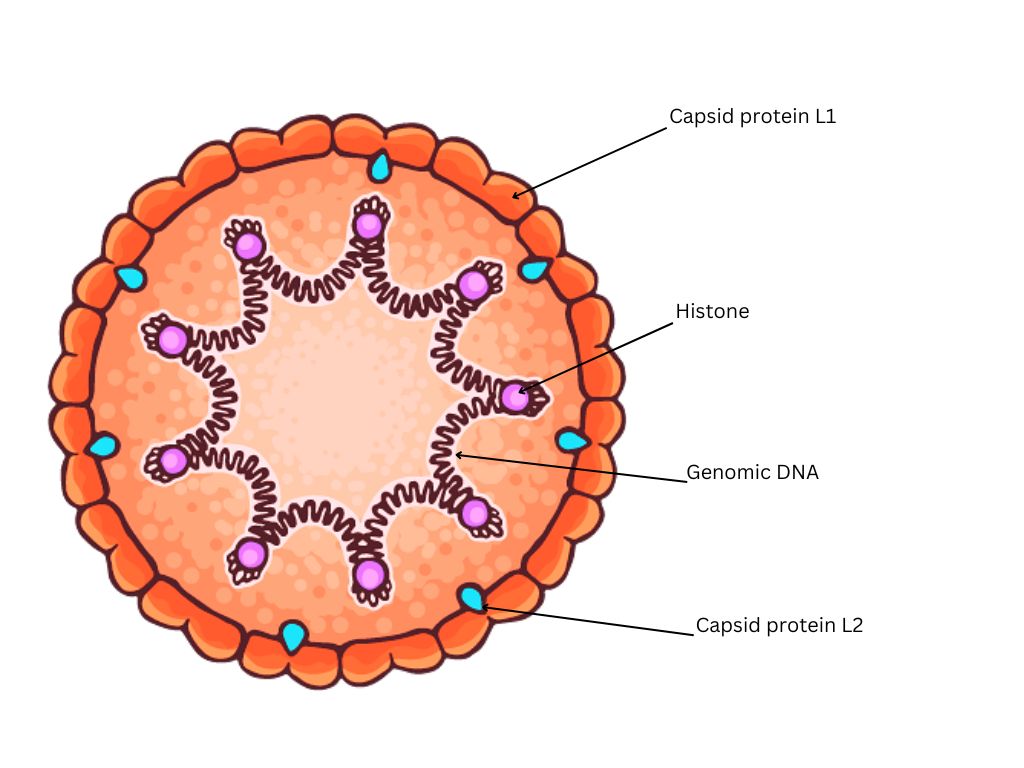
HPV viral particles have a double-stranded DNA molecule at the centre and a coating of protein (capsid) that contains two structural proteins (L1 and L2).
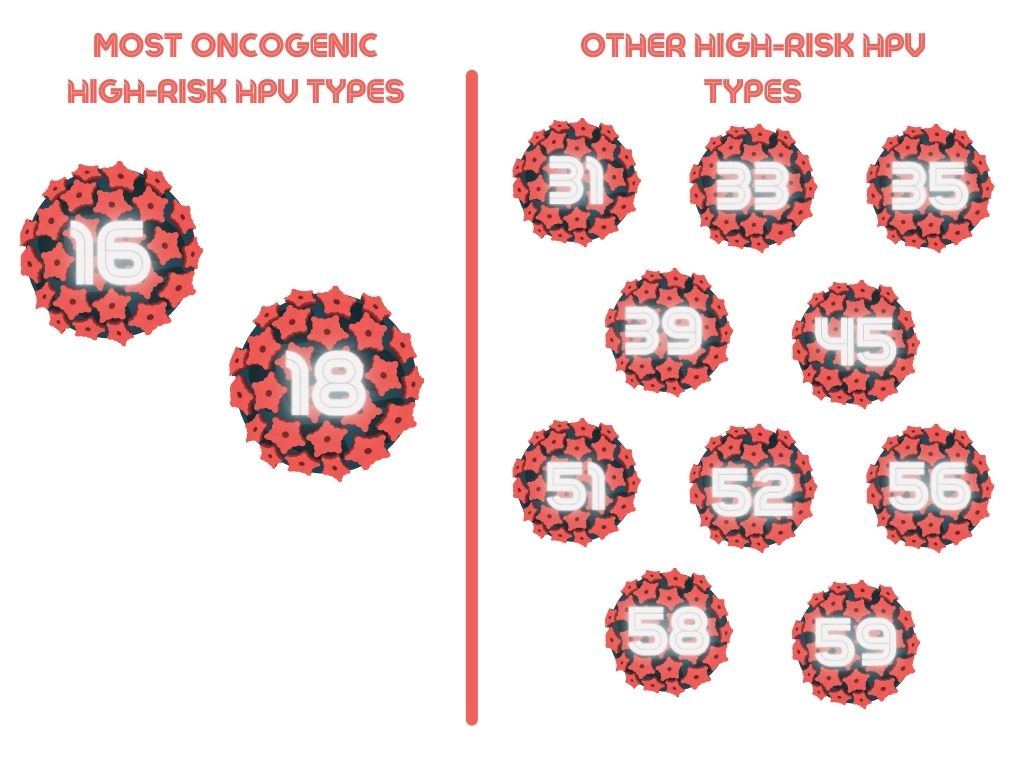
HPVs are categorized into different types according to their genetic makeup. Not all types are associated with cancer. There are 12 types of HPV that can cause cervical cancer and a few other cancer types (vulvar and vaginal cancers in women, penile cancer in men, and anal and oropharyngeal cancers in both sexes); these are called high-risk or oncogenic HPV types. Each type is known by a number, and the high-risk HPV types are HPV16, HPV18, HPV31, HPV33, HPV35, HPV39, HPV45, HPV51, HPV52, HPV56, HPV58, and HPV59. Of these, HPV16 and HPV18 are the most oncogenic. HPV16 and HPV18 are associated with nearly 70% of cervical cancers.
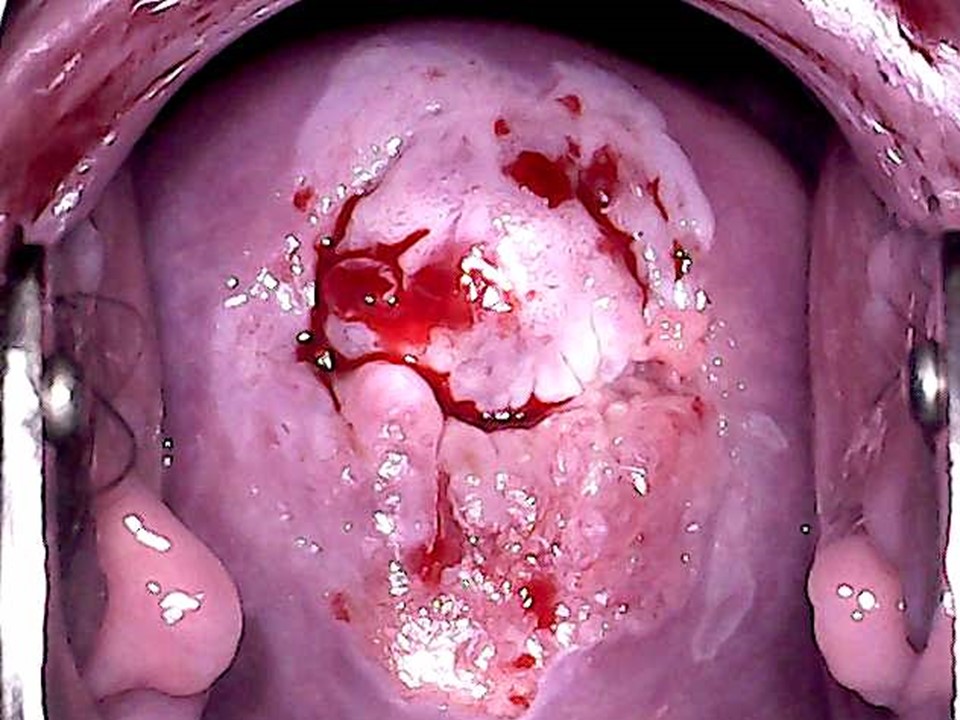
High-risk HPV infection is a necessary but not a sufficient cause of cervical cancer, because most women who develop the infection will not develop the cancer. There are co-factors that may increase the susceptibility of an individual woman to having persistent HPV infection, which may ultimately transform into malignancy. These co-factors include being infected at an early age, having multiple childbirths at an early age, smoking, HIV infection, other genital tract infections (Trichomonas vaginalis, Chlamydia trachomatis, and herpes simplex virus 2), and immunosuppression. Circumcision and regular use of condoms prevent viral transmission, although neither is 100% protective.
Two HPV types (HPV6 and HPV11) are responsible for nearly 90% of genital warts. Because HPV6 and HPV11 are not associated with any cancers, they are known as low-risk or non-oncogenic types. Click here to learn more about the genesis of cervical cancer via HPV infection |