Atlas of Colposcopy: Principles and Practice / Activity 6
Case |
Early and advanced cancers / Adenocarcinoma
Go back to the list
| Speculum examination |
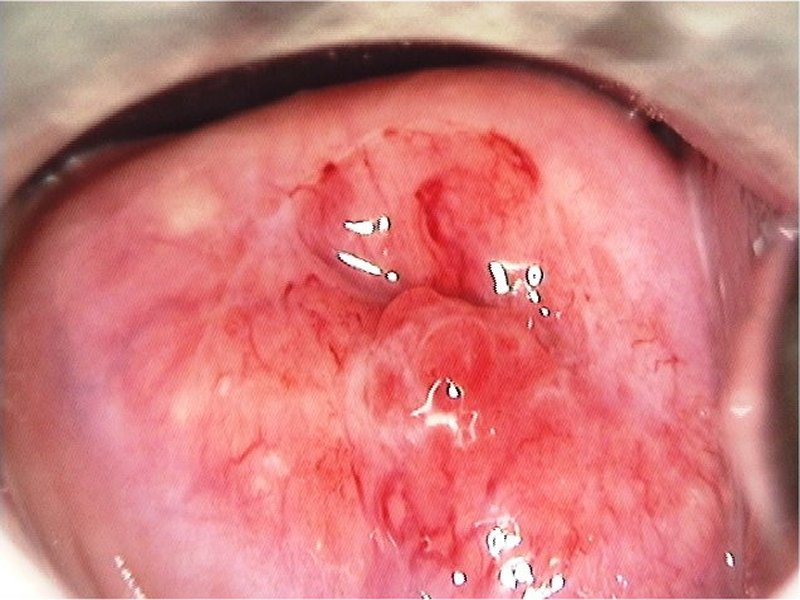
| After normal saline |
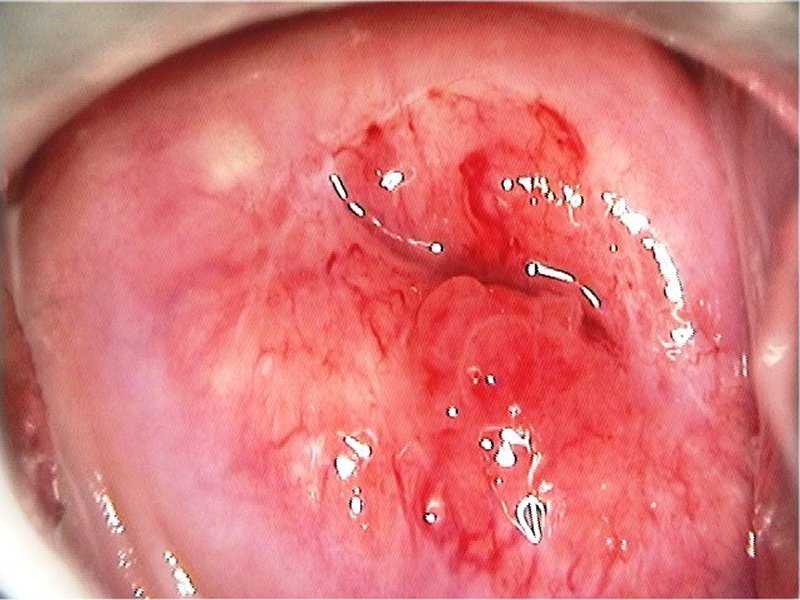
| After normal saline with green filter |
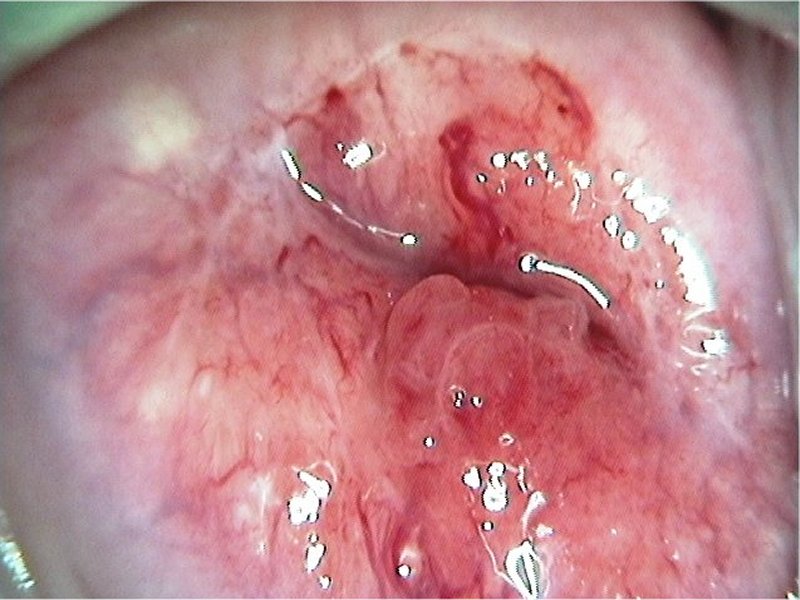
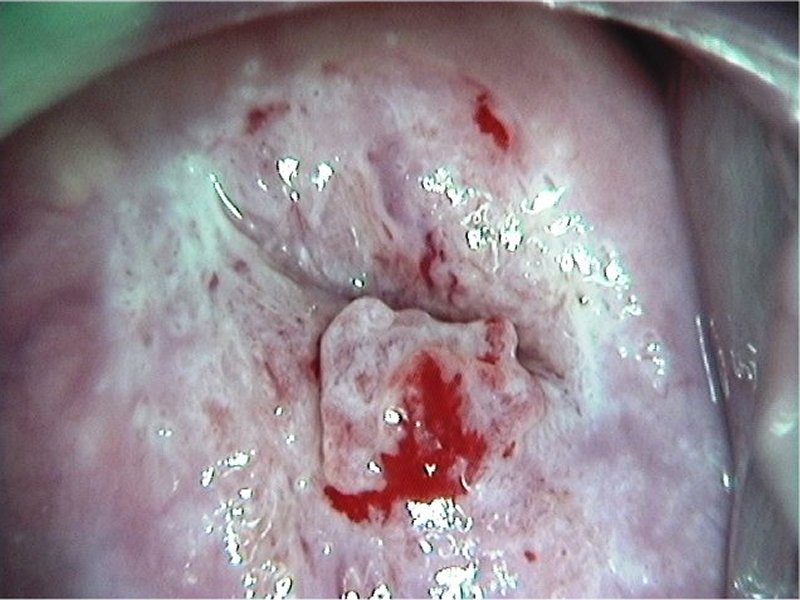
| After acetic acid |
| After acetic acid with green filter |
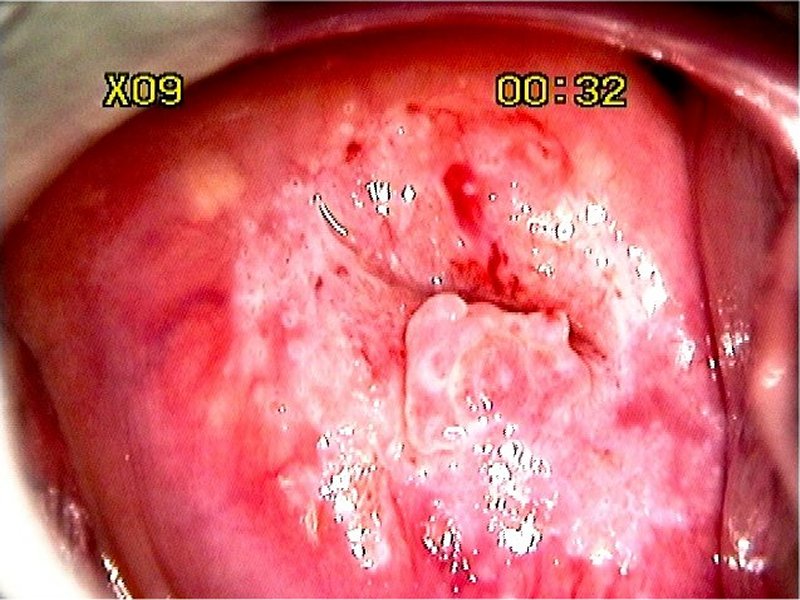
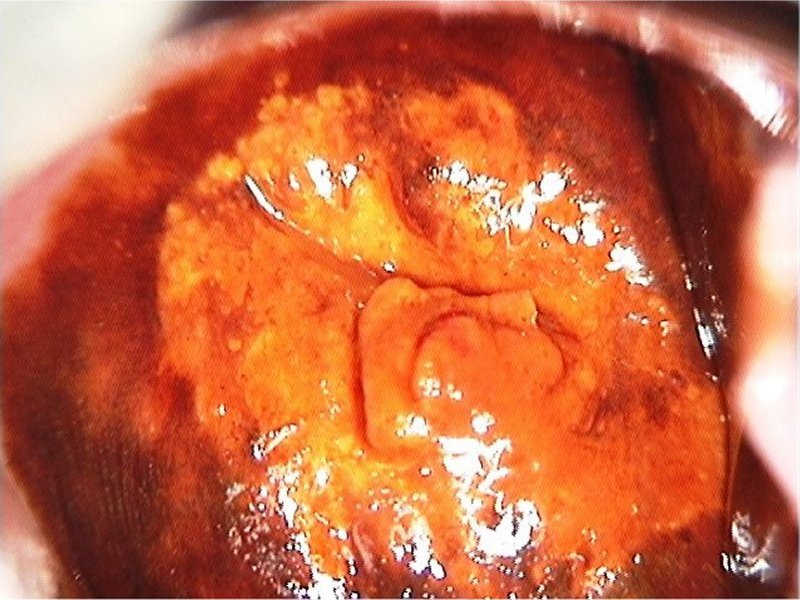
| After Lugolís iodine |
 General assessment General assessment | |||||||||||||||||
 Normal colposcopic findings Normal colposcopic findings | |||||||||||||||||
 Abnormal colposcopic findings Abnormal colposcopic findings | |||||||||||||||||
 General principles General principles | |||||||||||||||||
 Position and size Position and size | |||||||||||||||||
 Grade 1 (minor) Grade 1 (minor)
|  Grade 2 (major) Grade 2 (major)
|  Non-specific Non-specific
|  Suspicious for invasion Suspicious for invasion
|  Miscellaneous finding Miscellaneous finding
| |
Swede score:
| Nil or transparent | Thin, milky | Distinct, stearin | |
| Nil or diffuse | Sharp but irregular, jagged, satellites | Sharp and even, difference in level | |
| Fine, regular | Absent | Coarse or atypical vessels | |
| < 5 mm | 5-15 mm or 2 quadrants | >15 mm, 3-4 quadrants, or endocervically undefined | |
| Brown | Faintly or patchy yellow | Distinctly yellow |
Case Summary
| Provisional diagnosis: | Type 2 transformation zone; high-grade squamous intraepithelial lesion (HSIL) with suspected adenocarcinoma in situ. |
| Management: | LLETZ (type 3 excision) with endocervical curettage. Cold-knife conization can also be done. |
| Histopathology: | Adenocarcinoma in situ. |
| Comment: | Glandular lesions often coexist with high-grade squamous lesions. A dense acetowhite area over the columnar epithelium is characteristic of a glandular lesion. |