Using Human Papillomavirus (HPV) detection tests for cervical cancer screening and managing HPV-positive women – a practical guide / Activity 2
Anatomical considerations – Columnar epithelium | Click on the pictures to magnify and display the legends |
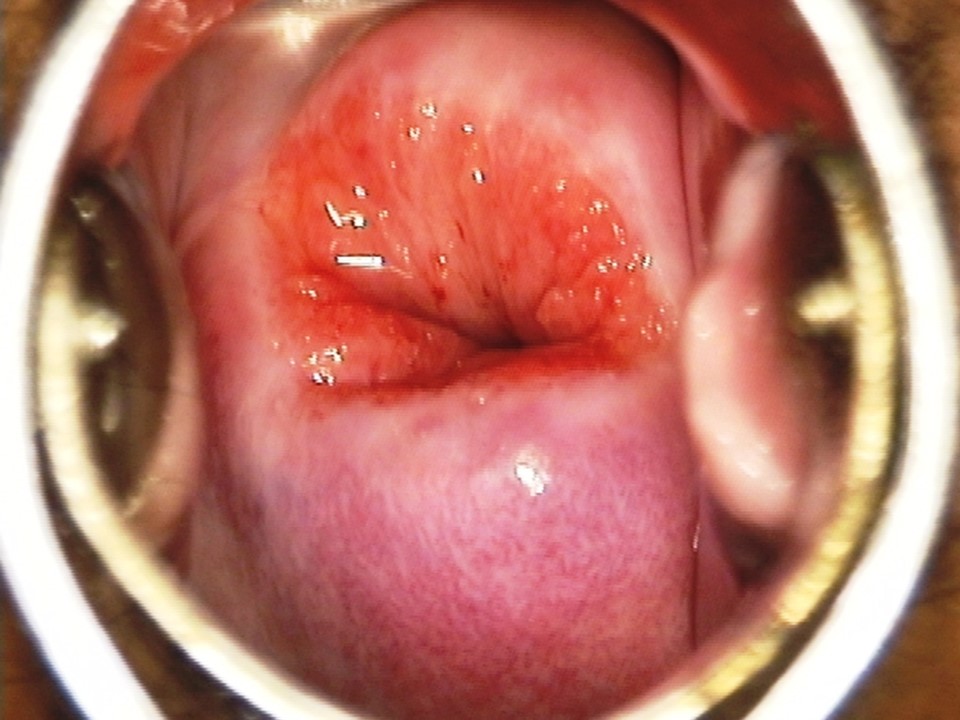
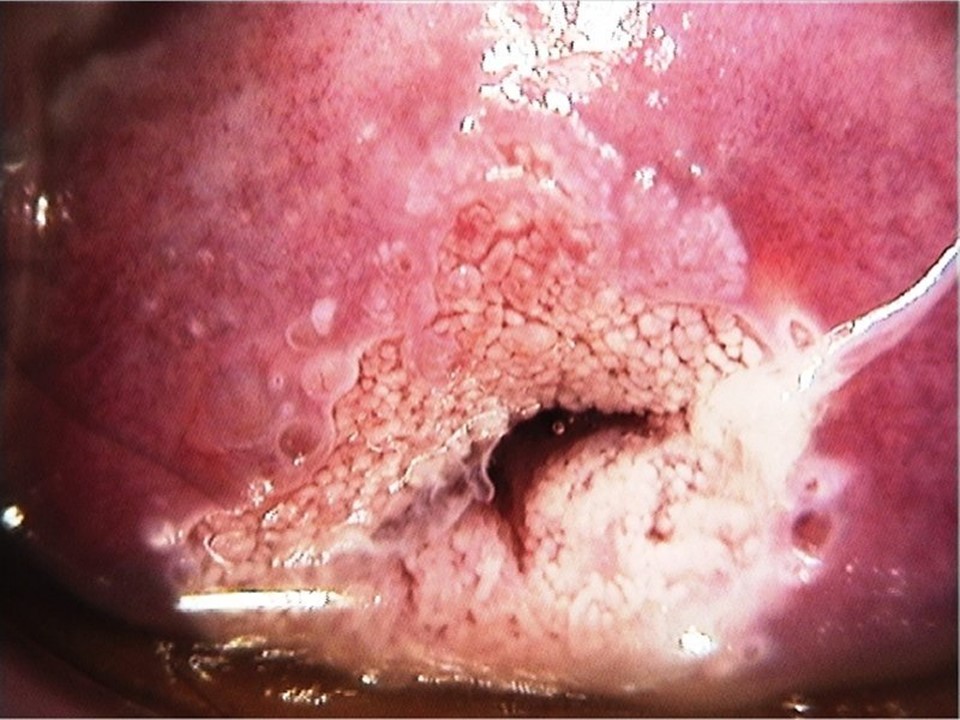
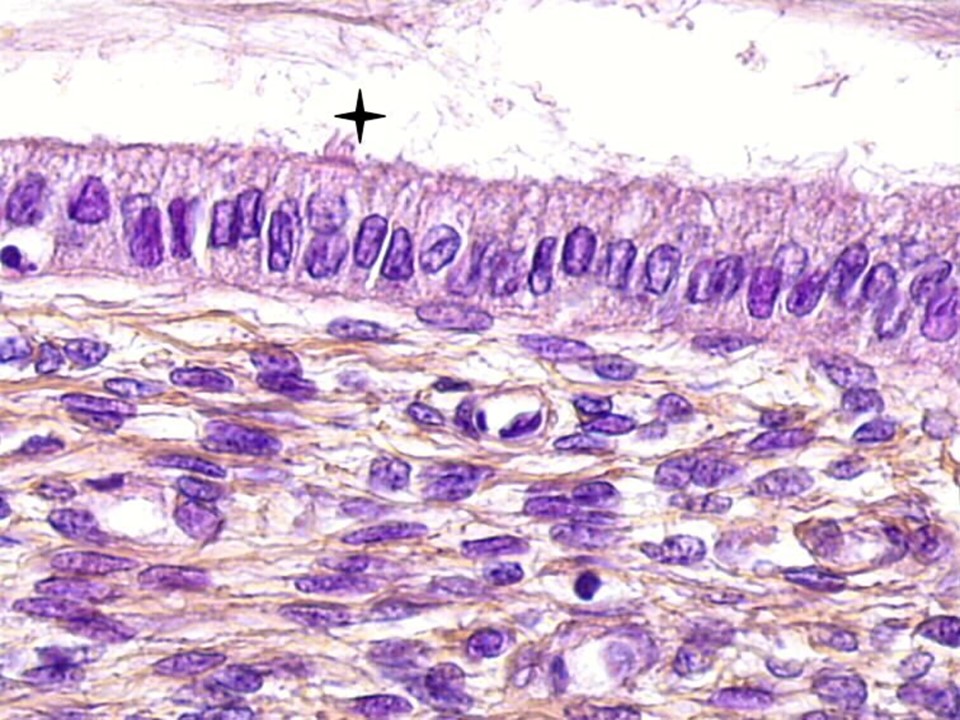
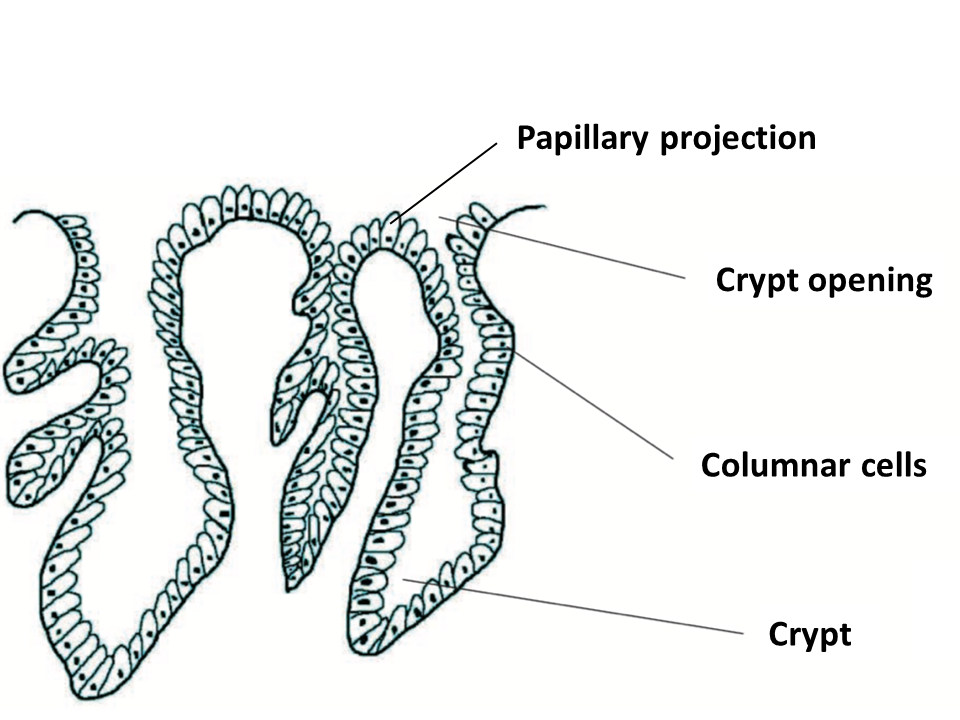
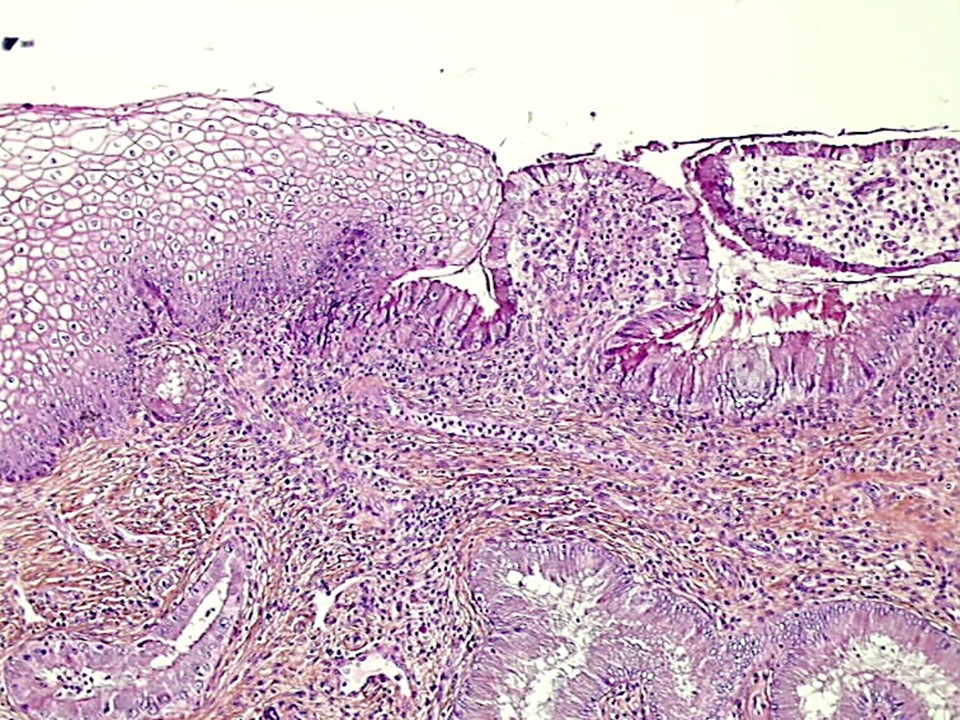
Naked-eye appearance of columnar epithelium On visual examination, the columnar epithelium is the most easily identifiable feature of the cervix. Because it is composed of only a single layer of cells, the blood vessels and stroma underneath are easily visible and give the endocervix a redder appearance. Light from the underlying cervical stroma is easily reflected through the thin epithelium, thus making the columnar epithelium appear strikingly red. The epithelium has a granular, velvet-like appearance because of the presence of papillary (finger-like) projections. Microscopic features of columnar epithelium The columnar epithelium is composed of a single layer of tall columnar cells that secrete mucin, which helps in the lubrication of the cervix and the vagina. The nucleus of each columnar cell is located close to the basement membrane. The columnar epithelium does not form a flat surface but is thrown into multiple folds in the lumen of the endocervical canal, giving rise to finger-like projections. These projections are called villi (singular-villus). The epithelium forms several invaginations into the cervical stroma, forming endocervical crypts. The depth of the crypts is 3–5 mm from the surface. The crypts are also known as glands. They open to the surface of the epithelium to discharge mucin, and the openings are called crypt openings. The next section discusses the squamocolumnar junction, a very important landmark on the cervix. |